689 views
Antonious Maria Selvam.S et al.: BIRT–HOGG–DUBE‘ Syndrome
Review Article
BIRT–HOGG–DUBE‘ Syndrome
Antonious Maria Selvam.S1, Praveen.R2, Yuvarajan.S3, and Kamal Barathi.S4
1, 2Assistant professor, 3Associate professor, 4Post graduate,
Sri Manakula Vinayagar Medical College & Hospital, Puducherry
Corresponding Author: Dr. Antonious Maria Selvam.S, Assistant professor, Sri Manakula Vinayagar Medical College & Hospital, Puducherry
How to cite this article: JAPT 2019:2(1):27-30
Historical Perspective:
Birt–Hogg–Dubé syndrome (BHD) is an inherited disorder characterised by multiplefibrofolliculomas, pulmonary cysts, pneumothorax, renal cysts and renal tumours. In 1977, Birt, Hogg and Dubé evaluated some members of Canadian family who presented them with thyroid cancers and found that they had similar type of fibrofollicular skin tumours with autosomal dominant inheritance.[1]The German dermatologists Hornstein and Knickenberg examined a middle-aged woman and her brother with multiple perifollicular fibromas and intestinal polyps and found that the disorder was probably inherited from their father who had bilateral renal cysts and unilateral lung cysts with skin tumours.[2] In 2001, two groups of investigators found the chromosomal location of the gene responsible for BHD following which Nickerson et al delineated the susceptibility locus of the gene on chromosome 17p11.2 and named as folliculin gene later.[3]
Climate change & Respiratory Health: A complex interaction
| Access this article online | |
| Quick Response Code: | Website: www.aptchest.com |
Clinical Manifestations:
Pulmonary Manifestations of BHD:
The common pulmonary presentation is spontaneous pneumothorax. Cystic lung lesions develop in early to mid-adulthood (30–40 years), but also described in patients ranging from 20 to 85 years. There is no gender predilection and there is no adequate studies about the role of cigarette smoking in development of cysts. Most of the patients (75 %) had recurrent pneumothorax. Toro et al. done a study on association of lung cysts, spontaneous pneumothorax and genetic relation in 89 families with Birt–Hogg–Dubé syndrome and indicated that presence of lung cysts was significantly associated with pneumothorax.[4] Hartman et al found incidental development of pulmonary adenoma and adenocarcinoma in FLCN heterozygous mice by regulation of Target of rapamycin complex 1 (TORC1). Further studies are warranted whether haploinsufficiency in FLCN predisposes to lung cancer.[5]
Dermatological Manifestations of BHD:
Skin lesions appears usually after 20 years of age which manifests as multiple, dome-shaped, whitish papules in the face. These lesions are seen mainly on the nose and cheeks, can be common on the neck, and sometimes on the trunk or the ears. Histologically, the skin tumours are benign hair follicle tumours designated as fibro-folliculoma. Birt and colleagues described fibrofolliculomas, trichodiscomas, and acrochordons as a triad of skin lesions that characterises BHD. Oral lesions may also occur in BHD. The diagnosis of BHD-associated skin lesions is based on both clinical presentation and histological examination.[6]
Renal Manifestations of BHD:
The most threatening complication of BHD is renal cancer. In serial studies by Pavlovich and colleagues, 34 of 124 individuals (27%) with BHD had renal tumours at a mean age of 50. However, the risk of renal cancer in BHD is uncertain forseveral reasons.[7] Firstly, identification of families with BHD has varied and was mostly based on dermatological signs. Secondly, the risk of renal cancer might not be the same for all BHD families. In particular, families in whom the pathogenic FLCN mutations have been described, lung cysts and pneumothorax were the only or predominant clinical manifestations. Based on current data, the risk of renal cancer should probably be considered the same for all carriers of FLCN mutations. Renal cancer is multifocal or bilateral in more than half of patients with BHD, which has implications for clinical management.
How to cite this article: Antonious Maria Selvam.S, Praveen.R, Yuvarajan.S, and Kamal Barathi.S, BIRT–HOGG–DUBE‘SYNDROME, JAPT 2019; 3:123-126
Diagnosis and Screening:
Genetic Testing:
FLCN is currently the only gene known to be associated with BHD. Detection of a pathogenic FLCN mutation not only confirms the diagnosis in the index patient but also allows presymptomatic testing of unaffected at-risk relatives. When a pathogenic mutation has been detected, cascade genetic testing aimed at identifying and counselling at-risk family members is indicated. Surveillance in FLCN-mutation carriers usually begins at the age of 20 years.
Radiologic Findings in BHD:
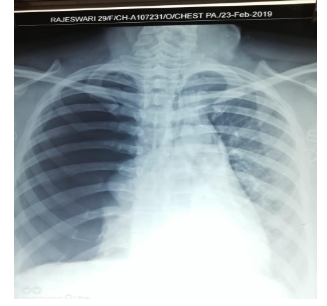
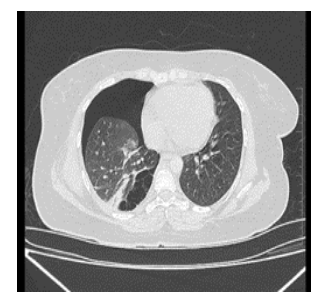
On CT thorax more than 80% of adult patients with BHD had multiple lung cysts with basal predominance. The characteristic chest CT findings of patients with BHD can be summarized as multiple, irregularly-shaped, thin-walled pulmonary cysts of various sizes, predominantly distributed to the lower medial and subpleural regions of the lung. The histology of pleuro pulmonary lesions in BHD has been studied in several patients and is consistent with emphysematous changes.
The lung parenchyma generally appears normal in patients with BHD. Despite the presence of multiplelung cysts, lung function is usually unaffected. Zbar and colleagues found a 50-fold increase in the risk of pneumothorax for BHD-affected individuals and this increase is probably related to the presence of lung cysts. Patients may have a single episode of spontaneous pneumothorax, but recurrent disease is more common.[8]
Criteria for Diagnosis:
DNA-based diagnosis of hereditary tumour syndromes has led to new classifications of these conditions based on the underlying gene defects.
Criteria proposed by the European Birt-Hogg-Dube Consortium:
Major Criteria
- At Least 5 fibrofolliculomas or trichodiscomas, at least 1 confirmed histologically, of adult onset
- Pathogenic germline mutation in FLCN
Criteria proposed by the European Birt-Hogg-Dube Consortium:
Major Criteria
- At Least 5 fibrofolliculomas or trichodiscomas, at least 1 confirmed histologically, of adult onset
- Pathogenic germline mutation in FLCN
Minor Criteria
- Multiple lung cysts: basally located with no other apparent cause, with or without spontaneous pneumothorax
- Renal cancer: early onset (
- First-degree relative with Birt-Hogg-Dube syndrome.
- Patients should fulfil 1 major or 2 minor criteria for diagnosis.
Management of BHD:
The Lungs
The management of BHD from a pulmonary perspective is largely focused on the approach to treatment of pneumothorax. The management of pneumothorax in patients with BHD differs from that recommended for primary spontaneous pneumothorax and is similar to that of LAM. In patients with primary spontaneous pneumothorax, the initial pneumothorax is usually managed with conservative measures (observation, aspiration, tube thoracostomy). Measures such as video assisted thoracoscopy (VATS) and mechanical or chemical pleurodesis are typically reserved for recurrent or non-healing cases. However, patients with BHD are at very high risk for recurrent pneumothorax.
Smoking is a known risk factor for development of primary spontaneous pneumothorax. Although no clear association has been found between smoking and the risk of pneumothorax in patients with BHD.[9] These patients should get regularly immunized. Pneumococcal vaccination and annual influenza vaccination should be strongly encouraged in patients with BHD. Currently, there is no evidence that patients with BHD should be advised against air travel.
The Skin
Treatment for skin fibrofolliculomas are limited. Case reports indicate that laser ablation using ND YAGor fractional CO2 laser is not curative, but gives temporary improvement. Pendulous fibrofolliculomas or skin tags can often be easily excised.
The Kidneys
Because of the increased risk of renal cancer, surveillance for renal tumours is indicated for carriers of FLCN germline mutations and for at-risk relatives in families with clinical BHD but without confirmed FLCN mutation. Currently, there are no established guidelines regarding surveillance for renal cancer in BHD. Lifetime screening is needed for individuals with BHD. Annual renal MRI seems to be the best available surveillance method, with high sensitivity and no radiation side-effects. If renal cancer is diagnosed, staging is done with standard procedures Treatment consists of nephron sparing surgery.
Conclusion
Respiratory specialists have a vital role in addressing climate change by communicating how climate change is a serious but remediable hazard to their patients.
Strategies to reduce impact of climate changes on health especially respiratory health are political in nature but citizens in particular health professionals must raise their voices in the decision process to give strong support for clean air policies at both national and international levels.
References
- Birt AR, Hogg GR, Dube WJ. Hereditary multiple fibrofolliculomas withtrichodiscomas and acrochordons. Arch Dermatol 1977;113:1674–7.
- Hornstein OP, Knickenberg M. Perifollicular fibromatosis cutis with polyps of thecolon: a cutaneo-intestinal syndrome sui generis. Arch Dermatol Res1975;253:161–75.
- Happle R. Hornstein-Birt-Hogg-Dube syndrome: a renaming and reconsideration. AmJ Med Genet A 2012;158A:1247–51.
- Schmidt LS, Warren MB, Nickerson ML, Weirich G, Matrosova V, Toro JR, Turner ML, Duray P, Merino M, Hewitt S, Pavlovich CP. Birt-Hogg-Dube syndrome, a genodermatosis associated with spontaneous pneumothorax and kidney neoplasia, maps to chromosome 17p11. 2. The American Journal of Human Genetics. 2001 Oct 1;69(4):876-82.
- Hartman TR, Nicolas E, Klein-Szanto A, Al-Saleem T, Cash TP, Simon MC, Henske EP (2009) The role of the Birt-Hogg-Dubé protein in mTOR activation and renal tumorigenesis. Oncogene 28:1594–1604
- Menko FH, Van Steensel MA, Giraud S, Friis-Hansen L, Richard S, Ungari S, Nordenskjöld M, Hansen T, Solly J, Maher ER, European BHD Consortium. Birt-Hogg-Dubé syndrome: diagnosis and management. The lancet oncology. 2009 Dec 1;10(12):1199-206.
- Pavlovich CP, Walther MM, Eyler RA, et al. Renal tumours in theBirt-Hogg-Dube syndrome. Am J SurgPathol2002; 26: 1542–52.
- Zbar B, Alvord WG, Glenn G, et al. Risk of renal andcolonic neoplasms and spontaneous pneumothorax in theBirt-Hogg-Dube syndrome. Cancer Epidemiol Biomarkers Prev2002;393–400.
- Ayo DS, Aughenbaugh GL, Yi ES, et al. Cystic lung disease inBirt-Hogg-Dube syndrome. Chest 2007; 132: 679–84.





