689 views
Dhanasekar et al.: An Interesting Case of Pneumocytoma In A 17-Year-Old Teenager
Case Report
An Interesting Case of Pneumocytoma In A 17-Year-Old Teenager
Dhanasekar1, Rajagopalan1, Shanmuga Priya1, Taanya Joseph1, Periyasamy2 and Ramkumar2
1Department of Chest & TB, 2Department of CTVS
Sri Ramachandra Institute of Higher Education and Research, Chennai
ABSTRACT:
Pneumocytoma is a rare benign neoplasm of the lung. Mostly, asymptomatic, the presentation is usually with an incidental lung mass on Chest X-ray (CXR), commonly a solitary pulmonary nodule. The Computed tomography (CT) is usually characterized by a well- defined juxta pleural mass and with probable calcification. The management of pneumocytoma includes limited resection, which is considered adequate. We report the case of a 17-year-old girl with complaints of shortness of breath for three months. On examination of the respiratory system, there were decreased movements, dullness to percussion and absent reath sounds in left hemithorax. CXR showed left opaque hemithorax. PET CT showed FDG (18F‐fluorodeoxyglucose) avid (Maximum standardized uptake value [SUV]= 14.53), eterogeneous mass lesion occupying the entire left lung. Initially misdiagnosed to be malignant due to the strong FDG uptake. CT guided biopsy was suggestive of spindle cell neoplasm. The patient was taken up for pneumonectomy under cardiopulmonary bypass due to adherence of mass to the left pulmonary artery. Postoperative histopathological examination was reported as benign pneumocytoma. Immunohistochemistry (IHC) panel of the lesion cells was reported strongly positive for vimentin, and focal strong positivity for both Thyroid transcription factor 1 (TTF1) and Epithelial membrane antigen (EMA). The patient is on follow up and is apparently doing well with no complications or recurrence.
Keywords: Benign tumour, Pneumocytoma, solitary pulmonary nodule.
Corresponding Author: Dr. Dhanasekar, Department of Chest, Sri Ramachandra Institute of Higher Education and Research
How to cite this article: Dhanasekar, Rajagopalan, Shanmuga Priya, Taanya Joseph, Periyasamy and Ramkumar, An Interesting Case of Pneumocytoma In A 17- Year-Old Teenager, JAPT 2019:2(1):36-39
Introduction
Pneumocytoma is a rare benign neoplasm of the lung with a female to male ratio of 5:1. Usually, asymptomatic and observed in the female during the fifth decade. Apparently, derived from and has a resemblance to pneumocytes and embryonic respiratory epithelium.1,2
Case Report
A 17-year-old girl presented with complaints of shortness of breath and non-productive cough for three months. Breathlessness was insidious in onset and progressive from grade II to grade III MMRC, non-productive cough. No history of loss of weight or appetite. No history was suggestive of fever, chest pain or dysphagia. Nothing significant was found on general physical examination. The respiratory system revealed central trachea and decreased movements on the left side and dullness to percussion and absent breath sounds in left hemithorax. On imaging, a chest x-ray showed left opaque hemithorax, trachea central.
| Access this article online | |
| Quick Response Code: | Website: www.aptchest.com |

Figure 1: Chest x-ray showing opaque lefthemithorax
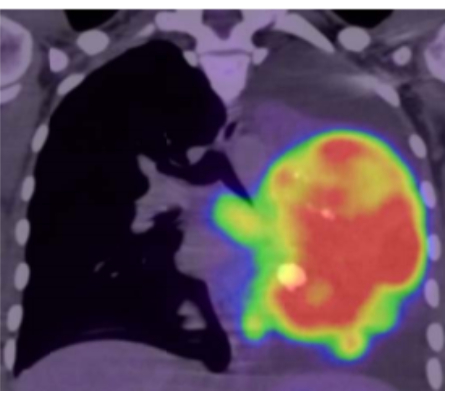

Figure 2 and 3: CT imaging of the chest showing heterogenous mass occupying the entire left lung


Figure 4 and 5: PET CT: axial view and coronal view of the thorax showing FDG avid heterogenous mass occupying the entire left lung
(Fig.1). Plain CT of the chest (Fig 2&3). PET CT (Fig 4&5) showed FDG avid (SUV max 14.53)
heterogeneous mass lession occupying the entire left lung (142 x 83 mm) and soft tissue density lesions along the parietal pleura, enlarged lymph nodes in prevascular and left supraclavicular regions
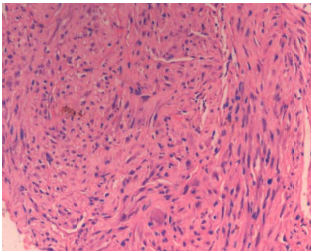
Figure 6: CT guided biopsy was suggestive of spindle cell neoplasm

Figure 7: Intraoperative mass
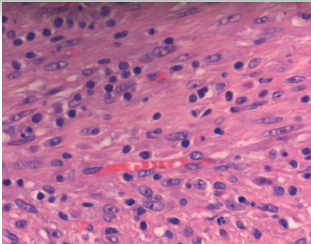
Figure 8: Histology of the lesion

Figure 9: Vimentin strongly positive

Figure 10: EMA: Focal strong positivity
Discussion
Pneumocytoma is a well-circumscribed lung parenchymal lesion and is characterised microscopically by a papillary pattern or islands filled with bland polygonal cells with abundant eosinophilic cytoplasm and indistinct cell borders. It was moved from “miscellaneous tumours” to “Adenomas” in 2015 WHO Classification. It’s historic misnomer “sclerosing hemangioma” originated from morphologic similarity to a dermatopathology lesion of the same name, now known as fibrous histiocytoma.3
This tumour is usually seen in females in the middle age. Most of the patients are asymptomatic. They usually have an incidental lung mass on chest radiograms. CT is characterized with well-defined juxta pleural mass.4 Calcification may often be seen almost, 41% of the tumours show calcification on microscopic evaluation5 Most of the pneumocytomas show increased FDG uptake (false positivity), with SUV max values significantly correlating with tumour size.6
Conclusion
Pneumocytoma is a rare benign neoplasm and one must not forget the importance of diagnosing
pulmonary pneumocytoma at the cytological level by identifying a dual cell population and preparing cell block for immunohistochemistry. It must always be considered in a middle-aged female with incidental lung mass/ solitary pulmonary nodule even if an FDG PET-CT indicates hypermetabolic malignancy.
REFERENCES
- Lim JH, Lee N, Choi DW, et al. Pulmonary sclerosing pneumocytoma mimicking lung cancer: Case report and review of the literature. Thorac Cancer 2016;7(4):508–511.
- Gupta M, Shah J, Manipadam M, Rao V. Case of pulmonary pneumocytoma: A probable
cytological diagnosis with histopathological confirmation. Indian Journal of Pathology and Microbiology 2014;57(1):89. - Travis WD, Brambilla E, Nicholson AG et al.The 2015 World Health Organization Classification of Lung Tumors: Impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol 2015; 10: 1243–1260
- Devouassoux-Shisheboran M, Nicholson AG, Leslie K, Niho S. Sclerosing hemangioma. In: Travis WD, Brambilla E, Müller-Hermelink HK, Harris CC, editors. World Health Organization Classification of Tumours: Pathology and Genetics of Tumours of the Lung, Pleura, Thymus and Heart. 1 st ed. Lyon: IARC Press; 2004. p. 115-7.
- Y.C. Cheung, S.H. Ng, J.W.C. Chang, et al.Histopathological and CT features of pulmonary sclerosing haemangiomas. Clin Radiol 2003; 58:630-5.
- Lim J, Lee N, Choi D, Oh H, Park H, Kim K et al. Pulmonary sclerosing pneumocytoma mimicking lung cancer: Case report and review of the literature. Thoracic Cancer. 2016;7(4):508-511.
- Miyagawa-Hayashino A, Tazelaar HD, Langel DJ, Colby TV. Pulmonary sclerosing hemangioma with lymph node metastases: report of 4 cases.Arch Pathol Lab Med 2003;127(3):321-5.
- Baysak A, Oz A, Moğulkoç N, Bishop P, Ceylan K. A rare tumor of the lung: Pulmonary sclerosing hemangioma (pneumocytoma). Respiratory Medicine. 2013;107(3):448-450.





