696 views
S. Priya et al.: A Case Report of Extramedullary Plasmacytoma – Presenting as a Chest Wall Tumour
Case Report
A Case Report of Extramedullary Plasmacytoma – Presenting as a Chest Wall Tumour
S.Priya1, Murugan2, Mahilmaran 2
1Department of Pulmonology, Vellore Medical College, Vellore
2Institute of Thoracic Medicine, Madras Medical College, Chennai.
Abstract
Plasmacytoma refers to a malignant plasma cell tumor growing within soft tissue or within the axial skeleton. Plasmacytoma accounts for six percent of all primary chest wall tumours. A solitary extramedullary plasmacytoma is reported three percent of plasma cell disorders. A 65 year male patient presented with complaint of swelling in the back of right side of the chest noticed for one month, pain over the swelling and dry cough for two weeks. Physical examination revealed a diffuse, lobulated swelling in the back of right side of chest which is firm to hard in consistency. The chest radiograph showed a large extra-pulmonary opacity with well-defined medial margin and lateral margin merging with chest wall on right side and blunting of the right costophrenic angle. The histopathological examination of tru-cut biopsy section showed fragments of fibrocartilagenous stroma infiltrated by mononuclear cells with round to oval nucleus and eosinophilic cytoplasm and some foci showed plasmocytoid features with the intervening stroma shows proliferating capillaries thereby features suggestive of plasmacytoma. The specimen is positive for CD 138 by the immunohistochemistry analysis which is the hallmark for diagnosing plasmacytoma.
Keywords: Extramedullary Plasmacytoma, Tru-cut biopsy, Immunohistochemistry..
Corresponding Author: Dr. S. Priya, Assistant Professor, Department of Pulmonology, Vellore Medical College, Vellore
Introduction
A plasmacytoma is a discrete, solitary mass of neoplastic monoclonal plasma cells in either bone or soft tissue (extramedullary). Plasmacytoma accounts for six percent of all primary chest wall tumours. There are three distinct groups of plasmacytoma defined by the International Myeloma Working Group1:
Solitary plasmacytoma of bone (SPB), Extramedullary plasmacytoma (EMP) and Multiple plasmacytoma that are either primary or recurrent. A solitary extramedullary plasmacytoma is reported three percent of plasma cell disorders and it presents without bony or systemic involvement.
In the United States, the incidence is approximately 0.15 cases/100,000 person-years accounting for approximately 450 new cases per
How to cite this article: S.Priya, Murugan, Mahilmaran, A Case Report of Extramedullary Plasmacytoma – Presenting as a Chest Wall Tumour, JAPT 2020; 3(1):47-52
year. The incidence is highest in Blacks and lowest in Asians and Pacific Islanders. Men are diagnosed twice as frequently as women. The median age at diagnosis is 55 to 65 years, which compares with a median age at diagnosis of 71 years for patients with multiple myeloma (MM) 2,3,4. SPB has been reported in patients as young as 15 years 4,5,6. Although an increased risk of plasma cell dyscrasia has been reported in first- degree relatives of patients with monoclonal gammopathy of undetermined significance and patients with multiple myeloma, there are no data on familial predisposition in solitary plasmacytoma.
The diagnostic criteria for solitary bone plasmacytoma (SBP) with the use of magnetic resonance imaging (MRI), flow cytometry, and polymerase chain reaction (PCR) are as follows, single area of bone destruction due to clonal plasma cells, bone marrow plasma cell infiltration not exceeding 5% of all nucleated cells, absence of osteolytic bone lesions or other tissue involvement (no evidence of myeloma), absence of anemia, hypercalcemia, or renal impairment attributable to myeloma, low concentration of serum or urine monoclonal protein and preserved levels of uninvolved immunoglobulins.
The diagnostic criteria for extramedullary plasmacytoma (EMP) are as follows ,tissue biopsy showing monoclonal plasma cell histology, bone marrow plasma cell infiltration not exceeding 5% of all nucleated cells, absence of osteolytic bone lesions or other tissue involvement (no evidence of myeloma),absence of hypercalcemia or renal failure and a low serum M protein concentration.
Case Report
A 65 year male patient presented with complaint of swelling in the back of right side of the chest one month and pain in the swelling and dry cough for past two weeks. The painless swelling is noticed by the patient before one month which is insidious in onset and slowly progressive in size. The dull aching pain started later over the swelling brought the patient to seek medical help. The patient complained of shortness of breath and wheeze. He denied trauma to the chest wall. He was a former smoker with pack years of 20, consumes alcohol daily since 20 yrs of age and betal nut chewer. Physical examination revealed a diffuse, lobulated swelling in the back of right side of the chest which was firm to hard in consistency, not mobile, not tender, no warmth and no dilated veins over the swelling, not fixed to the skin extending from inferior angle of scapula to posterior right costal margin approximately 20 x10 cm in size. On auscultation breath sound decreased in intensity in right infrascapular and infra axillary areas. The biochemical markers are normal. The ultrasonogram of the chest showed right pleural effusion and diagnostic thoracentesis proved to be exudative effusion The chest radiograph showed a large extra- pulmonary opacity with well-defined medial margin and lateral margin merging with chest wall on right side and blunting of the right costo phrenic angle. The contrast enhanced chest computed tomogram feature was a large homogenous enhancing soft tissue mass lesion in right prevertebral region with large exophytic chest wall component and dural component causing widening right neural foramina in fifth and sixth thoracic vertebra with mass effect on posterior aspect of right lung with right pleural effusion. Fine needle aspiration cytology reported by pathologist as cellular smear showing predominantly singly dispersed round to oval cells with moderate amount of cytoplasm and eccentrically placed nuclei, numerous binucleated, multinucleated cells with numerous mitotic figure suggestive of Plasmacytoma. The histopathological examination of tru-cut biopsy section showed fragments of fibrocartilagenous stroma infiltrated by mononuclear cells with round to oval nucleus and eosinophilic cytoplasm and some foci showed plasmocytoid features with the intervening stroma shows proliferating capillaries thereby features suggestive of Plasmacytoma. The specimen is positive for CD 138 by the immunohistochemistry analysis which is the hallmark for diagnosing Plasmacytoma.

Picture of the case showing swelling in the back
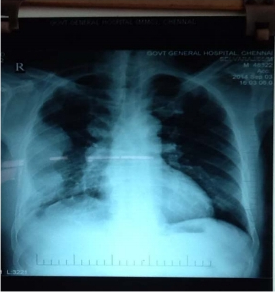
Figure 2 – Chest radiograph of the case
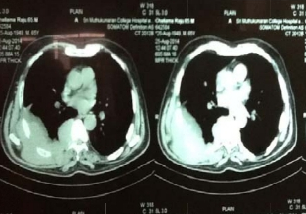
Figure 3 – Chest Computed tomograph of the case
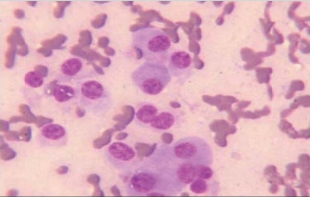
Figure 4 – Fine needle aspiration cytology section showing round to ovel cells with moderate amount of cytoplasm and eccentrically placed nuclei
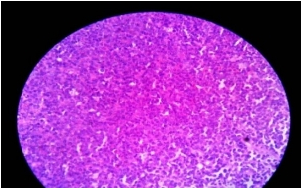
Figure 5 – Sectioo to tru cut biopsy specimen fibrocartilagenous stroma infiltrated by mononuclear cells with round to oval nucleus and eosinophilic cytoplasm
Bone marrow biopsy section showed bony trabaculae with intervening normocellular marrow showing myeloid erthroid precursors and adequate megakaryocte. No evidence of multiple myeloma in the material, Urine Bence jones protien was negative. The urine protien electrophoresis showed M – band.The serum protein electrophoresis revealed paraprotein band which is present in the gamma region.Thus the solitary extramedullary plasmacytoma is diagnosed in this case.
Treatment
Radiotherapy is the main choice of treatment for both solitary plasmacytoma of bone and extramedullary plasmacytoma, and local control rates of >80% can be achieved. This form of treatment can be used with curative intent because plasmacytoma is a radiosensitive tumor. Surgery is an option for extramedullary plasmacytoma, but for cosmetic reasons it is generally used when the lesion is not present within the head and neck region. NCCN guidelines – Primary solitary plasmacytoma treatment for Osseousis local radiotherapy, for extraosseous radiotherapy followed by surgery, adjuvant chemotherapy may be considered for patients with tumours larger than 5 cm. In this patient, proteosome inhibitor Inj. Bortezomib and T.Lenalidomide,an anti-tumor drug that has been shown to interact with ubiquitin E3 ligase cereblon enzyme inside the tumor cell was given, patient improved symptomatically with reduction in size of tumor with two cycles of chemotherapy and and its mass effect on the right lung is revealed.

Figure 6: Post Chemotherapy

Figure 7: Post chemotherapy – Chest Radiography
Discussion
The diagnosis of plasmacytoma uses a diverse range of interdisciplinary techniques including serum protein electrophoresis, bone marrow biopsy, urine analysis for Bence Jones protein and complete blood count, plain film radiography, MRI and PET-CT.8,9
Serum protein electrophoresis separates the proteins in the serum to analysis the antibodies. Normal blood serum contains a range of antibodies and are said to be polyclonal, whereas serum from a person with plasmacytoma may show a monoclonal spike. This is due to an outgrowth of a single type of plasma cell that forms the plasmacytoma and produces a single type of antibody. The plasma cells are said to be monoclonal and the excessively produced antibody is known as monoclonal protein or paraprotein.11 Paraproteins are present in 60% of solitary bone plasmacytoma and less than 25% of extramedullary plasmacytoma.
Bone marrow biopsies are performed to ensure the disease is localised; and in solitary plasmacytoma of bone or extramedullary plasmacytoma there will not be an increase of monoclonal plasma cells which is similar in this case as there is no evident of multiple myeloma
in the bone marrow biopsy. Tissue biopsies of solitary plasmacytoma of bone and extramedullary plasmacytoma are used to assess the phenotype of the plasma cells. Histological analyses can be performed on these biopsies to see what Cluster of differentiation (CD) markers are present and to assess monoclonality of the cells. CD markers can aid in the distinction of extramedullary plasmacytoma from lymphomas. In our patient, CD 138 is positive which is the pathognomic for plasmacytoma.
Skeletal surveys are used to ensure there are no other primary tumors within the axial skeleton. MRI can be used to assess tumor status and may be advantageous in detecting primary tumors that are not detected by plain film radiography. PET-CT may also be beneficial in detecting extramedullary tumours in individuals diagnosed with SPB. CT imaging may be better than plain film radiography for assessing bone damage.8,9
An important distinction to be made is that a true plasmacytoma is present and not a systemic plasma cell disorder, such as multiple myeloma. The difference between plasmacytoma and multiple myeloma is that plasmacytoma lacks increased blood calcium, renal insufficiency, anemia and multiple bone lesions (collectively termed CRAB).The reported patients’ blood calcium and renal function are normal as well as blood hemoglobin level of 11.5 gm%.
As mentioned in the reference articles11,12, for the distinction from solitary bone plasmacytomain extramedullary plasmacytoma there is the presence of only one lesion (either in bone or soft tissue), normal bone marrow (<5% plasma cells), normal skeletal survey, absent or low paraprotein and no end organ damage which was found in the present case. Most cases of solitary plasmacytoma of bone progress to multiple myeloma within 2–4 years of diagnosis, but the overall median survival for solitary plasmacytoma of bone is 7–12 years. 30– 50% of extramedullary plasmacytoma cases progress to multiple myeloma with a median time of 1.5–2.5 years. 15–45% of SPB and 50–65% of extramedullary plasmacytoma are disease free after 10 years.12
Conclusions
In this case bone marrow biopsy and immunochemistry report of CD 138 positive ruled out the diagnosis of multiple myeloma and confirmed the diagnosis of extramedullary
plasmacytoma, hence patient treated with chemotherapy and outcome is satisfactory. Any patient in the median age group of 55 presenting with soft tissue swelling with no skeletal involvement, early suspicious and diagnosis of benign form of tumor can be treated with neo- adjuvant chemotherapy.
References
1. International Myeloma Working Group (June 2003). “Criteria for the classification of monoclonal gammopathies, multiple myeloma and related disorders: a report of the International Myeloma Working Group”. Br. J. Haematol. 121 (5): 749–57.
2. Dores GM, Landgren O, McGlynn KA, et al. Plasmacytoma of bone, extramedullary plasmacytoma, and multiple myeloma: incidence and survival in the United States, 1992-2004. Br J Haematol 2009; 144:86.
3. Shih LY, Dunn P, Leung WM, et al. Localised plasmacytomas in Taiwan: comparison between extramedullary plasmacytoma and solitary plasmacytoma of bone. Br J Cancer 1995; 71:128.
4. Frassica DA, Frassica FJ, Schray MF, et al. Solitary plasmacytoma of bone: Mayo Clinic experience. Int J Radiat Oncol Biol Phys 1989; 16:43.
5. Pavithran K, Doval DC, Rao CR, et al. Pediatric solitary plasmacytoma. Acta Oncol 1997; 36:83.
6.Boos N, Goytan M, Fraser R, Aebi M.et al Solitary plasma- cell myeloma of the spine in an adolescent. Case report of an unusual presentation. J Bone Joint Surg Br 1997; 79:812.
7. Greenberg AJ, Rajkumar SV, Vachon CM.et al Familial monoclonal gammopathy of undetermined significance and multiple myeloma: epidemiology, risk factors, and biological characteristics. Blood 2012; 119:5359.
8. Kilciksiz S, Karakoyun-Celik O, Agaoglu FY, Haydaroglu A (2012).et al “A review for solitary plasmacytoma of bone and extramedullary plasmacytoma”. Scientific World Journal. 2012:895765.
9. Dimopoulos M, Terpos E, Comenzo RL, et al. (September 2009). “International myeloma working group consensus statement and guidelines regarding the current role of imaging techniques in the diagnosis and monitoring of multiple Myeloma”. Leukemia. 23 (9): 1545–56.
10. O’Connell TX, Horita TJ, Kasravi B (January 2005).et al “Understanding and interpreting serum protein electrophoresis”. Am Fam Physician. 71 (1): 105–12.
11. M. Hughes; R. Soutar; H. Lucraft; R. Owen; J. Bird et al. “Guidelines on the diagnosis and management of solitary plasmacytoma of bone, extramedullary plasmacytoma and multiple solitary plasmacytomas.
12. Weber DM (2005). “Solitary bone and extramedullary plasmacytoma”. Hematology Am Soc Hematol Educ Program: 373–6.





