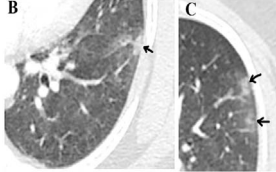
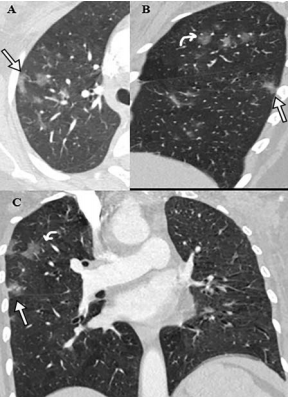
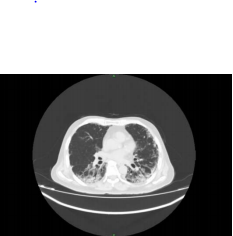
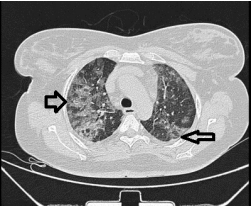
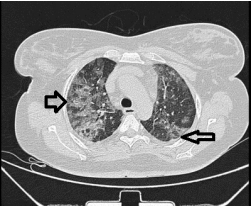
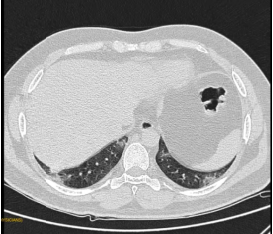
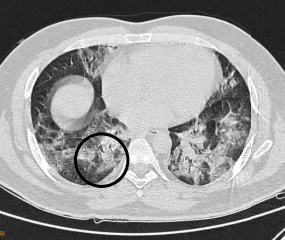
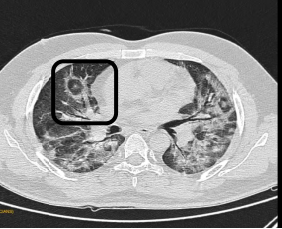
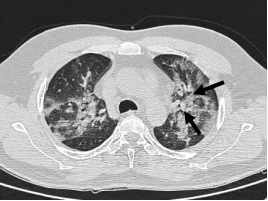
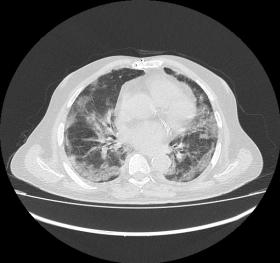
Fig 3: CT Axial section through lower lobes showing multiple coalescing areas of ground glass opacities in peripheral and peribronchovascular distribution bilaterally
Treatment
Patient was transferred to dedicated COVID ICU and was treated with intravenous Remdesivir 200 mg on day 1 followed by 100 mg once daily for total of 5 days. She was continued on supplemental oxygen, methyl prednisolone (40mg/day) was continued for total of 10 days in view of extensive pulmonary involvement.Oral hydroxychloroquine was stopped in view of QT prolongation.
Outcome and Follow-UP
Patient improved clinically with the treatment given and her oxygen requirement gradually decreased over next 48 – 72 hours. She was weaned off oxygen and shifted to ward. As she was maintaining saturation on room air for the next around 48 hours in ward without any new symptoms, she was discharged and advised to follow home quarantine for 2 weeks.
Discussion
The Novel coronavirus is a single stranded, enveloped, positive sense RNA virus which is transmitted between humans mainly by airborne droplets, direct contact and feco-oral route (5, 6, 7). The symptom complex of COVID-19 is non-specific – most commonly presenting with fever, fatigue, dry cough, myalgia and dyspnea. Though the diagnosis can be suspected based on combination of detailed history (including contact, travel, geography etc.),symptomatology and radiology, the confirmation of the disease is reliably made by laboratory diagnosis (5).
Though a variety of immunological and serological laboratory tests are available for COVID 19, RT PCR is the gold standard test recommended for confirmation of SARS CoV-2 by WHO (7). Serological tests are not recommended for acute infection settings as it is less likely to yield a positive result during initial period of infection (8).
The COVID-19 RT-PCR is a real-time reverse transcription polymerase chain reaction test which detects nucleic acids of SARS CoV-2 qualitatively in recommended respiratory specimens, either upper or lower, collected appropriately from a suspected individual. But the test is plagued with documented false-negative results even in patient with typical clinical and radiological presentation (9) and it has been recommended that a single negative RT PCR should not be taken as a rule-out test for the diagnosis of COVID 19 in a strongly suspicious patient, as in our patient (10).
A Meta-analysis including five studies (957 patients) has reported upto 29% rate of initial false negative RT-PCR (11). The factors that can be causing such false-negativity were attributed to virus related factors such as RNA sequences variation , genomic mutations, viral load kinetics; host related factors such as early presentation, viral tropism to infect lower respiratory tract and procedure related factors such as inappropriate collection, transportation or laboratory facilities (12). There are case reports with multiple false-negative RT-PCR results in COVID – 19 patients (13, 14). Though,bronchoscopy with lavage has been recommended in suspcious cases with negative RT-PCR of nasopharyngeal sample, it has procedure related risk for patient with respiratory failure. The option was discussed with our patient but she was not willing for it and wanted to get repeat upper nasopharyngeal sampling.
The role of CT imaging of thorax in such situations of false negative NAAT has been emphasized by many investigators. In a study done by Xie et al, which included 167 laboratory confirmed COVID 19 patients, had high concordance of CT positivity with RT-PCR positivity – 93%. But significantly 5 patients(3%), had CT positivity with negative RT-PCR on initial testing who became positive on subsequent testing within 2 – 8 days (8).Another retrospective study of 34 patients with confirmed COVID 19, 10 symptomatic patients who had initial negative RT PCR had typical CT imaging findings suggesting the disease (15). Another study of 51 patients done in China showed CT imaging to have significantly superior sensitivity compared to RT-PCR test –98% to 71% (16). A study of 82 patients showed comparable sensitivity of CT chest (77%) and RT-PCR (79%) but a comprehensive strategy of combining the two modality improved sensitivity to 94% (17). Li et al (4) showed in a retrospective study of 53 patients, CT thorax has very low rate of missed diagnosis (3.8%).
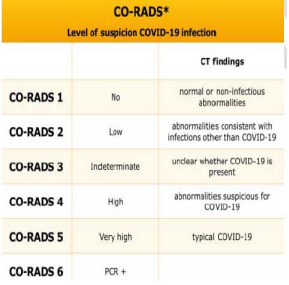
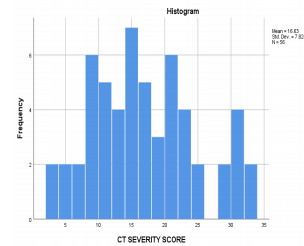
Apart from the role in diagnosis of the disease, CT thorax has been shown to be helpful in screening asymptomatic individuals,assessing response to disease, prognosticate the disease (CT severity score) (18, 19). The CO-RADS (COVID-19 Reporting and Data System), a categorical reporting system which assesses the degree of pulmonary involvement by COVID-19 on chest CT in patients with moderate to severe symptoms with categories 1 to 5 according to increasing suspicion on CT (20). CT severity score, a scoring assigned out of 25 according to percentage of involvement of 5 lobes, correlates with severity of the disease and helps prognosticate (21).
WHO has provided important Infection prevention and control checklist to be followed for acquisition of CT in a suspected or confirmed patient (22).
The role of CT has been clearly proven to be beneficial in high clinical suspicion scenario with negative initial RT-PCR test and of those with CT findings typical of COVID 19, a repeat RT-PCR testing [as per local governmental /institutional policy (ideally between 1 – 7 days)]should be performed (13, 14).
Learning Points/Take Home Messages 3-5 bullet points
- RT-PCR for SARS CoV-2, the current Gold-Standard test, has sensitivity of around 70%and can yield false negative result even in a typical COVID – 19 pneumonia.
- RT – PCR can be taken as a good Rule-in test but it should not be considered as a single Rule-out test for the diagnosis of COVID -19.
- CT thorax, though non-specific, has good sensitivity and has very low rate of missed diagnosis of COVID – 19 pneumonia.
- CT thorax should be done in patients with high clinical suspicion but negative RT-PCR testing and among those who have typical CT features, repeat PCR testing should be done.
References
1. https://www.who.int/news-room/detail/29-06-2020-covidtimeline
2. https://www.indiatoday.in/india/story/kerala-reports-first-confirmed-novel-coronavirus-case-in-india-1641593-2020-01-30
3. Weissleder R, Lee H, Ko J, Pittet MJ. COVID-19 diagnostics in context. Science Translational Medicine. 2020;12(546).
4. Li Y, Xia L. Coronavirus Disease 2019 (COVID-19): Role of Chest CT in Diagnosis and Management. American Journal of Roentgenology. 2020;214(6):1280–6.
5. He, F, Deng, Y, Li, W. Coronavirus disease 2019: What we know? J Med Virol. 2020; 92: 719–725. https://doi.org/10.1002 /jmv.25766
6. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al.Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus–Infected Pneumonia. New England Journal of Medicine. 2020;382(13):1199–207.
7. C. Li, C. Zhao, J. Bao, B. Tang, Y. Wang, B. Gu,Laboratory Diagnosis of Coronavirus Disease-2019 (COVID-19), Clinica Chimica Acta (2020), doi: https://doi.org/10.1016/j.cca.2020.06.045
8.https://www.uptodate.com/contents/coronavirus-disease-2019-covid-19-diagnosis?topicRef=126981&source=related_link#H2813503854
9. Xie X, Zhong Z, Zhao W, et al. Chest CT for Typical 2019-nCoV Pneumonia: Relationship to Negative RTPCR Testing. Radiology. 2020 Feb 12. doi: 10.1148/radiol.2020200343
10. BMJ 2020;369:m1808
11. Arevalo-Rodriguez I, Buitrago-Garcia D, SimancasRacines D, et al. False-negative results of initial RT-PCR assays for COVID-19: a systematic review. April 21,2020
(https://www.medrxiv.org/content/10.1101/2020.04.1
6.20066787v1. opens in new tab). preprint.
12. Tahamtan, A., & Ardebili, A. (2020). Real-time RT-PCR in COVID-19 detection: issues affecting the results. Expert review of molecular diagnostics, 20(5),453–454.
https://doi.org/10.1080/14737159.2020.1757437
13. Feng H, Liu Y, Lv M, Zhong J. A case report of COVID19 with false negative RT-PCR test: necessity of chest CT. Japanese Journal of Radiology. 2020;38(5):409–10.
14. Lagziel T, Quiroga L, Ramos M, Hultman CS, Asif M. Two False Negative Test Results in a Symptomatic Patient with a Confirmed Case of Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) and Suspected Stevens-Johnson Syndrome/Toxic Epidermal Necrolysis (SJS/TEN). Cureus. 2020;
15. Chen, H. J., Qiu, J., Wu, B., Huang, T., Gao, Y., Wang, Z.P., Chen, Y., & Chen, F. (2020). Early chest CT features of patients with 2019 novel coronavirus (COVID-19) pneumonia: relationship to diagnosis and prognosis. European radiology, 1–8. Advance online publication. https://doi.org/10.1007/s00330-020- 06978-4
16. Fang Y, Zhang H, Xie J, Lin M, Ying L, Pang P, et al.Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology. 2020;:200432.
17. He, J. L., Luo, L., Luo, Z. D., Lyu, J. X., Ng, M. Y., Shen,X. P., & Wen, Z. (2020). Diagnostic performance between CT and initial real-time RT-PCR for clinically suspected 2019 coronavirus disease (COVID-19)patients outside Wuhan, China. Respiratory medicine, 168, 105980. https://doi.org/10.1016/j.rmed.2020.105980
18. Tenda ED, Yulianti M, Asaf MM, et al. The Importance of Chest CT Scan in COVID-19. Acta Med Indones.2020;52(1):68-73.
19. Tabatabaei SMH, Talari H, Moghaddas F, Rajebi H.Computed Tomographic Features and Short-term Prognosis of Coronavirus Disease 2019 (COVID-19) Pneumonia: A Single-Center Study from Kashan, Iran.Radiology: Cardiothoracic Imaging. 2020;2(2).
20. Prokop M, Everdingen WV, Vellinga TVR, Ufford JQV, Stöger L, Beenen L, et al. CO-RADS – A categorical CT assessment scheme for patients with suspected COVID19: definition and evaluation. Radiology. 2020;:201473.
21. https://japi.org/w2f4d464/clinico-radiologicalevaluation-and-correlation-of-ct-chest-images-withprogress-of-disease-in-covid-19-patients#abstract
22. World Health Organization. (2020). Use of chest imaging in COVID-19: a rapid advice guide, 11 June 2020 (No. WHO/2019-nCoV/