694 views
Sridhar R et al.: Early Onset Chyliform Pleural Effusion-A Rare Case
Case Report
Early Onset Chyliform Pleural Effusion-A Rare Case
Sridhar R1, Rajeswari P2, Mahilmaran A2
1Department of Respiratory Medicine – Apollo Hospitals, Chennai.
2Department of Thoracic medicine – Madras Medical College, Chennai.
Abstract
Chyliform pleural effusion is turbid or milky from high lipid content without cholesterol crystals. Chyliform
pleural effusion is a rare presentation than chylous or pseudochylous pleural effusion. The mean duration of
the effusion to turn chyliform is 5 years. A 20 year old male presented with dry cough, left side chest pain and
dyspnea on exertion and gives history of bilateral pleural effusion for which he had taken empirical
antituberculous treatment. Chest radiograph showed bilateral pleural effusion more on left side. Thoracentesis
done on left side revealed milky white coloured fluid with elevated cholesterol levels and Mycobacterium
tuberculosis was detected and was not resistant to Rifampicin in cartridge based nucleic acid amplification
test[CBNAAT] for pleural fluid. Contrast enhanced CT chest showed healed fibrotic lesion in bilateral upper
lobe with bilateral pleural effusion with thickened pleura on left side. Patient diagnosed as chyliform effusion
and treated with Intercostal drainage and antituberculous treatment. Less than 200 cases of chyliform have
been reported in the medical literature of which microbiologically confirmed tuberculous chyliform effusion is
rarely reported. Chyliform effusion rarely develops within one year and Tuberculosis presenting as Chyliform
pleural effusion is a rare phenomenon.
Keywords: chyliform effusion, CBNAAT, tuberculosis
Corresponding Author: Dr.Sridhar R, Department of Respiratory Medicine – Apollo Hospitals, Chennai.
How to cite this article: Sridhar R,Rajeswari P, Mahilmaran A, Early Onset Chyliform Pleural Effusion-A Rare Case, JAPT 2019 2(2):76-79
Introduction
Pseudochylothorax is a cholesterol-rich
pleural effusion that is commonly associated with chronic inflammatory disorders such as tuberculosis or rheumatoid arthritis1. Pleural fluid is milky or at least turbid and it persists after centrifugation, due to a high lipid content of the pleural fluid. High levels of lipid accumulate in the pleural fluid in two conditions. First, when the thoracic duct is disrupted, chyle can enter the pleural space to produce a chylous pleural effusion.
Second, pseudochylothorax is high cholesterol content and milky pleural fluid often with cholesterol crystals seen on microscopy. Chyliform pleural effusion is turbid or milky from high cholesterol content without cholesterol crystals2. Chyliform pleural effusion is a rare presentation than chylous or pseudochylous pleural effusion.
Less than 200 cases have been reported in the medical literature of which microbiologically confirmed tuberculous chyliform effusion is rarely reported. The etiology is tuberculosis in 54% of
Case Report
A 20 year old male engineering student, smoker presented with dry cough, left side chest pain and dyspnea on exertion and gave history of empirical antituberculous treatment one month before for clinically diagnosed tuberculous bilateral pleural effusion. Patient gave the history of straw coloured fluid on pleural aspiration seven months before in some other hospital and pleural fluid reports were not available. On examination patient
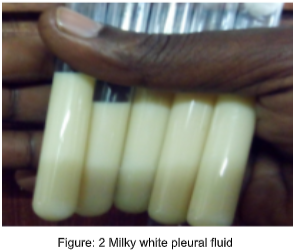
was conscious, oriented, comfortable at rest, general examination was normal, stony dullness and decreased breath sounds on left infrascapular & infraaxillary area. Other system examination was normal. Chest radiograph showed bilateral pleural effusion more on left side, USG confirmed the same. Diagnostic thoracentesis revealed milky white coloured fluid and it was sent for analysis which showed
- Triglycerides elevated (224mg/dl)
- Cholesterol elevated (324mg/dl) levels
- Cholesterol crystals -negative
- CBNAAT –Mycobacterium tuberculosis detected, Rifampicin resistant not detected.
- Pleural fluid culture both aerobic and anaerobic—no growth
- Pleural fluid AFB smear-negative
Serum lipid profile:
- Cholesterol-150
- Triglycerides-80
- HDL-23
- Pleural fluid cholesterol to triglyceride ratio >1
- Pleural fluid cholesterol to serum
- cholesterol ratio >1
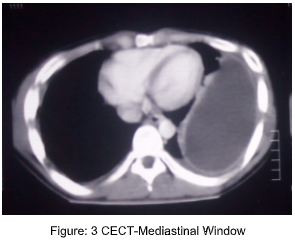
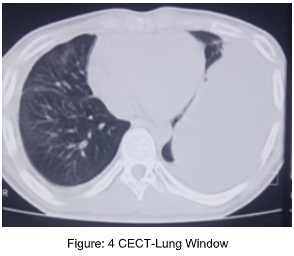
Contrast enhanced CT chest showed healed fibrotic lesion in bilateral upper lobe with bilateral pleural effusion and thickened pleura on left side. Bronchoscopy was done no abnormality was found in the tracheobronchial tree, bronchial wash for CBNAAT was negative. Contrast enhanced CT abdomen was normal and Rheumatoid factor was negative.
Tube thoracostomy was done on left side which drained 500 ml of milky white fluid and antituberculous treatment started according to RNTCP guidelines and thorcostomy tube was removed after drainage stopped and
symptomatically improved.


Discussion
Milky turbid pleural fluid can be due to chylothorax, pseudochylothorax or empyema. Milky turbid fluid does not clear on centrifugation can be either chylothorax or pseudochylothorax but in empyema, it clears due to sedimentation of cellular debris. In our case it was not clear on centrifugation so it was probably either chylothorax or pseudochylothorax2 . Milky pleural fluid with high triglycerides level favours chylothorax and high cholesterol level favours pseudochylothorax5 , in our case both were elevated. To further differentiate between these two we applied the ratio of pleural fluid triglycerides to pleural fluid cholesterol which was <1, ratio of serum cholesterol to pleural fluid cholesterol also 2 . Radiologically, thickened pleura was also more suggestive of pseudochylothorax than chylothorax because chyle is non-irritant, chylothorax is usually not associated with pleural thickening or loculation 1 . Some authors mentioned cholesterol crystals negative pseudochylothorax as chyliform effusion2 . In our case elevated pleural fluid cholesterol, thickened pleura and negative cholesterol crystals favoured the diagnosis of chyliform effusion.
When a patient is diagnosed as a chyliform pleural effusion, the possibility of tuberculosis should always be entertained. In our case, CBNAAT of chyliform fluid confirmed tuberculosis. The diagnosis and therapeutic decision may be difficult in tuberculous pseudochylothorax. In the review of the literature by Garcia-Zamalloa et al., Ziehl-Neelsen stain was positive in only two cases, levels of adenosine deaminase correlated with infectious activity in 40% of those tested, and M. tuberculosis was isolated in 14% (11% of pleural fluid cultures and 17% of pleural biopsy cultures) 3 . The polled sensitivity of CBNAAT in pleural fluid was 51.4% and specificity was 98.6% 9 . So far no study has been published on sensitivity of CNNAAT in chyliform fluid. This is the first case report of CBNAAT positive chyliform pleural effusion
The mean duration of the effusion to turn chyliform is 5 years. Only 9% of patients with pseudochylothorax developed in pleural effusion of less than 5 years’ duration 4 ; the most frequent cause was parasitic infection followed by rheumatoid arthritis 6, 7 , carcinoma of the lung 8 . In our case chyliform effusion developed within one year which was very rare. So far only one case of tuberculous pseudochylothorax developing in a pleural effusion of less than one years’ evolution has been reported4.
Antituberculosis treatment is recommended for patients with pseudochylothorax in which M. tuberculosis is isolated, in culture-negative patients with a history of past tuberculosis, and in purified protein derivative–positive patients with progressive effusions 3 . Decortication should be considered in chyliform effusion if the patient is symptomatic and the underlying lung is believed to be functional. In our case the patient improved with intercostal drainage and Antituberculosis treatment.
Conclusion
Milky pleural fluid with pleural thickening should consider pseudochylothorax than chylothorax which needs to be confirmed by biochemical analysis. The ratio of pleural fluid triglycerides to pleural fluid cholesterol suggestive of pseudochylothorax even triglycerides level elevated above normal. Chyliform effusion rarely develops within one year and Tuberculosis presenting as chyliform pleural effusion is a rare phenomenon which should be kept in mind in non-resolving pleural effusion with thickened pleura especially in high prevalence country like India.
References
1. Wrightson JM, Stanton AE, Maskell NA, Davies RJO, Lee YCG. Pseudochylothorax without pleural thickening: time to reconsider pathogenesis?. Chest. 2009;136(4):1144‐1147.
2. Light RW. Chylothorax and pseudochylothorax. In: Light RW, ed. Pleural Diseases. 3rd ed. Baltimore, MD: Williams& Wilkins; 1995:284–298.
3. Garcia-Zamalloa A, Ruiz-Irastorza G, Aguayo FJ, et al.Pseudochylothorax: report of 2 cases and review of the
literature. Medicine (Baltimore). 1999;78:200–207
4. Nogueras C, Monteagudo M, Vila M, Cabezuelo A,Mariscal D, Berlanga E. Recent-onset tuberculous pleurisy
presenting as pseudochylothorax. Am J Med2002;113:166-8.
5. Vaz MA, Teixeria LR, Vargas FS, Carmo AO, AntonangeloL, Onishi R, et al. Relationship between pleural fluid and serum cholesterol levels. Chest 2001;119:204-10.
6. Carel RS, Schey G, Bruderman I. Chyliform Pleural Effusion: An Unusual Manifestation of Hepatothoracic Echinococcus Cysts. Chest. 1975 Oct 1;68(4):598-9.
7. Muresan C 1 , Muresan L 2 , Grigorescu I 1 , Dumitrascu DL 1 Lung India. Chyliform effusion without pleural thickening in a patient with rheumatoid arthritis: A case report. 2015 Nov-Dec;32(6):616-9.
8. Goldman A, Burdorf TH. Cholesterol pleural effusion: a report of three cases with a cure by decortication. Dis
Chest. 1950;18: 586–594.
9. Sehgal IS, Dhooria S, Aggarwal AN, Behera D, Agarwal R. 2016. Diagnostic performance of Xpert MTB/RIF in tuberculous pleural effusion: systematic review and meta-analysis. J Clin Microbiol 54:1133–1136.





