Amal Johnson et al.: Prevalence of Prediabetes and Diabetes in 100 Newly Diagnosed Adult Asthmatics who Visited Pulmonology…
Prevalence of Prediabetes and Diabetes in 100 Newly Diagnosed Adult Asthmatics who Visited Pulmonology OPD of A Tertiary Care Hospital in South India – A Cross Sectional Study
Amal Johnson1, Mobeen Quadri2,Sumi M Sam3, Narasimhan R4
1Post Graduate, Department of Respiratory Medicine, Apollo Hospitals, Greams Road, Chennai, India
2Post Graduate, Department of Respiratory Medicine, Asram Medical College, Eluru, Andhra Pradhesh, India
3Physician Assistant, Department of Respiratory Medicine, Apollo Hospitals, Greams Road, Chennai, India
4Senior Consultant Pulmonologist, Apollo Hospitals, Greams Road, Chennai, India.
Abstract
Background: Diabetes mellitus is the most common endocrine disease and characterized by increased blood glucose levels. Diabetes has been associated with accelerated lung function decline, decrease in respiratory muscle strength altered bronchial reactivity. Methodology: This is a cross sectional study done in 100 consecutive patients >=18 years who visited Pulmonology OPD of Apollo Hospitals, Chennnai with respiratory symptoms and diagnosed to have asthma based on Spirometry according to GINA (2020) guidelines from March 2019 to May 2019. All patients with informed consent were subjected to serum HbA1C testing. Results: The results of HbA1C testing were as follows : 45 patients had HbA1C less than 5.6, 50 patients had HbA1C between5.6 to 6.4 which is classified as prediabetes and 5 patients had HbA1C greater than 6.4 which is classified as diabetes according to recent American diabetes association(ADA) guidelines. Conclusion:? There is a definite association of pre diabetes and diabetes with asthma and the drop in lung function correlates with the control of diabetes.
Keywords: Diabetes, Asthma, HbA1c, Prevalence.
Corresponding Author: Dr. Narasimhan R, Senior Consultant Department of Respiratory Medicine. Email:drrnarasimhan@gmail.com
How to cite this article: Amal Johnson, Mobeen Quadri, Sumi M Sam, Narasimhan R, Prevalence of Prediabetes and Diabetes in 100 Newly Diagnosed Adult Asthmatics who Visited Pulmonology OPD of A Tertiary Care Hospital in South India – A Cross Sectional Study, JAPT 2019; 2(3):94-99
Introduction
Diabetes mellitus (DM) comprises a group of metabolic disorders that share the common feature of hyperglycemia. DM is currently classified on the basis of the pathogenic process that leads to hyperglycemia. Type 1 DM is characterized by insulin deficiency, whereas type 2 DM is a heterogeneous group of disorders characterized by variable degrees of insulin resistance, impaired
insulin secretion, and excessive hepatic glucose production1,2. The global prevalence of DM is around 8.5% according to World Health Organization (2014)3. 366 million people will have DM by the year 2030. It is estimated that about In India, the prevalence is around 11.8%4. DM is a disease of significant morbidity and mortality in long term.
The diagnostic criteria for DM according to American Diabetes Association (ADA) include any one of the following5:
- Fasting plasma glucose ≥7.0 mmol/L (≥126mg/dL)
- Symptoms of diabetes plus a random blood glucose concentration ≥11.1 mmol/L (≥200mg/dL)
- 2-h plasma glucose ≥11.1 mmol/L (≥200mg/dL) during a 75-g oral glucose tolerance test.
- Hemoglobin A1c >6.5%
Prediabetes is an intermediate state of hyperglycemia with glycemic parameters above normal but below the diabetes threshold. It is defined as fasting blood glucose levels between 110mg/dl to 125mg/dl or HbA1C between 5.6 to 6.4%6.
HbA1C is glycosylated hemoglobin formed by non enzymatic addition of sugar to N-terminal of B chain which forms a Schiff base and converted into a Amadori product7. The use of HbA1C as a biomarker for monitoring the levels of glucose among diabetics was first proposed by Koenig et al8. It is a reliable measure of chronic glycemia and correlates well with the risk of long term diabetes complications. It is a convenient test, not requiring the patient to fast and uses only a single blood sample.
The metabolic, hormonal and microvascular disturbances frequently lead to kidney, retina, nerve and cardiovascular complications especially in uncontrolled DM. The damage to lungs resulting from chronic hyperglycemia has been studied recently and it occurs both in Type 1 and Type 2 DM.
The following complications are associated with DM1:
- Increased lung infection
- Pulmonary edema
- Sleeping respiratory disorders
- Reduced lung elasticity
- Decreased CO diffusion
- Altered bronchial reactivity
- Increased risk of thromboembolism
- Higher prevalence of pulmonary hypertension
The pathogenesis is related to the accumulation of advanced glycation end products in the alveolar basement membrane and oxidative stress9.
In patients with DM, there is histopathological evidence of thickened alveolar, epithelial and pulmonary capillary basal lamina10.
This study is an elementary attempt to estimate the prevalence of Prediabetes and Diabetes in newly diagnosed adult asthmatics.
Review of Literature
In the Framingham Heart study conducted on 3,254 participants, both FEV1 and FVC were lower in diabetics than in non-diabetics11.
In the COPD Gene study conducted with 10,129 participants, people with DM have reduced lung function after confounding for other known risk factors12.
In the Fremantle Diabetes Study done by Davis et al, there is an accelerated decline of FEV1 by 71ml/year and this decline related to poor glycemic control13.
In the Copenhagen City Heart Study conducted by Lange et al, FEV1 and FVC were consistently lower in diabetics, with a average reduction of 8% of the predicted value14.
The third national health and nutrition examination survey (NHANES III) conducted in 2005 over 1480 adults showed that there is a decrease of FEV1 and FVC in diabetics and the rate of decline associated with glycemic control15.
In meta analysis conducted by Borst et al on Diabetic pneumopathy, it is shown that lung function of diabetics is significantly impaired with 5% of predicted and correlates with glycemic state16..
In study entitled “Prevalence of bronchial asthma in patients with type 2 diabetes mellitus” by Themeli et al, 13.3% of the patients diagnosed to have diabetes had bronchial asthma17.
In an Australian retrospective, longitudinal cohort study done by Ehrlich et al, it is shown that the diabetics have increased risk of asthma (Hazard
ratio 1.08)18.
In cohort study conducted by Mueller et al entitled “ Asthma and the risk of type 2 diabetes in Singapore Chinese Health study” , asthma was associated with 31% increased risk of incident diabetes19.
In the sixth Korea National Health and Nutrition Examination Survey done by Kyung Hee Lee et al, the probability of asthma occurrence was 1.02 times higher20.
Objectives
To estimate the prevalence of Prediabetes and Diabetes in newly diagnosed adult asthmatics.
Materials and Methods
INCLUSION CRITERIA: Patients >=18 years diagnosed with Asthma based on spirometry according to GINA (2020) guidelines from March 2019 to May 2019 -FEV1 >=12% and 200ml.
EXCLUSION CRITERIA: Patients were excluded if age group <=18 or having other primary lung disease or already diagnosed to have diabetes.
Methodology :
This is a cross sectional study done in 100 consecutive patients >=18 years who visited Pulmonology OPD of Apollo Hospitals, Chennnai with respiratory symptoms and diagnosed to have asthma based on basis of variable symptoms (cough / wheeze / breathing difficulty / chest tightness) +/- reversible airflow limitation (spirometry – FEV1 > 12% and 200ml) according to GINA (2020) guidelines21 from March 2019 to May 2019. Demographic and clinical data collected
including Age, Gender, BMI, personal history of allergies (allergic rhinitis/atopic dermatitis), family history of asthma/allergies, smoking history, occupation history, history of respiratory infections and history of co morbidities and drug history. All patients with informed consent were subjected to
serum HbA1C testing.
Results
There were 70 males and 30 females in the study. The age range was between 19 to 58 and the average mean age was 35. The average BMI was 23 and 11 patients had BMI of >=30.
In patients with asthma, childhood history of allergy was present in 35% of patients and family history of asthma present in 35% of patients.
15 patients were smoking currently and 2 were former smokers. 3 patients had history of treated tuberculosis in the past.
In regard to co morbidities, 17 patients had systemic hypertension, 10 patients had underlying coronary artery disease, 4 patients had hypothyroidism and 3 patients had chronic kidney disease.
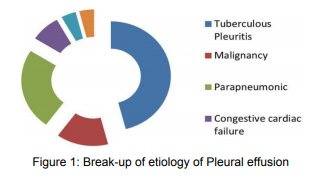
The results of HbA1C testing were as follows : 45 patients had HbA1C less than 5.6, 50 patients ad HbA1C between5.6 to 6.4 which is classified as prediabetes and 5 patients had HbA1C greater than 6.4 which is classified as diabetes according to recent American diabetes association(ADA) guidelines22.


The mean FEV1 of our patients was 64% and the mean bronchodilator reversibility was around 13%.
Out of the diagnosed as diabetes (HbA1C >- 6.5), 4 had moderate to very severe airflow obstruction in spirometry according to ATS/ERS 2005 classification23 , 24 out of 50 patients having prediabetes (HbA1C 5.6 -6.5) had moderate to very severe airflow obstruction in spirometry and 10 patients with HbA1C < 5.6 had moderate to very severe airflow obstruction in spirometry./p>

Discussion
There were 70 males and 30 females in the study and the sex ratio is 7:3. This is in discordant with the study results of Sofie et al24 where sex ratio of adult asthmatics diagnosed is 5:7. The average mean age was 35. This is in concordant with the study by Mirabelli et al.25 where the average age of
iagnosis in adult asthma is 38.
The average BMI was 23 kg/m2– Males with mean BMI of 24kg/m2 and Females with mean BMI of 23kg/m2. 11 patients had BMI of >=30 out of which 7 were females. This is in concordance with study done by Hjellvik et al.26 where the mean BMI in males was 26.2kg·m−2) than in females (24.7 kg·m−2), but severe obesity (BMI of ≥35kg kg·m−2) was more common in females than in males.

In patients with asthma, childhood history of asthma in 40% of patients, history of atopy in 70% of patients and family history of asthma present in
35% of patients. This is in concordance with the results of Moore et al.27.
But according to Siegal et al, there exists no relationship between atopy and development of diabetes mellitus and infact Cardwell et al. in their study have shown an inverse relationship between atopy and diabetes mellitus.
15 patients were smoking currently and 2 were former smokers. This is lesser than the prevalence of smoking in asthmatics is around 25% according to Parasuramalu et al.31 Also, asthmatic smokers are more prevalent for diabetes mellitus according to Song et al. due to exaggerated chronic inflammation.
In regard to comorbidities, 17 patients had systemic hypertension, 10 patients had underlying coronary artery disease, 4 patients had hypothyroidism and 3 patients had chronic kidney disease. This is in concordance with the study done by Xinming Su et al32. and Lee KH et al.20 where the most common co morbidity associated with asthma is hypertension. The possible pathway involved in development of hypertension in asthmatics is endothelin dysfunction and abnormal contraction of myosin II.
The results of HbA1C testing were as follows : 45 patients had HbA1C less than 5.6, 50 patients had HbA1C between 5.6 to 6.4 which is classified as prediabetes and 5 patients had HbA1C greater than 6.4 which is classified as diabetes according to recent American diabetes association(ADA) guidelines.
This prevalence of prediabetes among asthmatics in our study is 50% and is much more compared to our Indian prevalence of diabetes mellitus which is 14% according to Ramachandran et al33.
Also, the prevalence of diabetes among asthmatics in our study is 5% and is lesser than Indian prevalence of diabetes mellitus which is 11.8% according to Anjana RM et al.4
The prevalence of asthma and DM has been shown to range from 5% to 16% according to studies done by Adams et al34 and Caughey et al35 which correlates with our study.
The mean FEV1 of our patients was 64% and all patients had significant bronchodilator eversibility(>12% and 200ml). This is lesser than in study conducted by Sundeep Salvi et al.36 the mean FEV1 in diabetics was 78%.
The mean bronchodilator reversibility in diabetic asthmatics was 13% which is lesser than the mean of 21.5% in asthmatics according to Enrico Effler et al.37 which negatively correlates with asthma outcome.
We observed that 4 out of 5 patients had moderate to severe airflow obstruction who had HBA1C >=6.5%. and this is in concordance with study by Lee KH20 who showed that diabetics with higher HbA1C have increased risk of asthma occurence and poor asthma control.
According to Mueller et al38, possible mechanisms for increased risk of diabetes among asthmatics is
- unregulated expression of
proinflammatory pathways , including IL6, TNF-Alpha, adhesion molecules through activation of NF-KB - Hypoxia and intermittent hypoxia resulting in altered glucose metabolism via insulin dependent and insulin independent mechanisms
- Exposure to glucocorticoids as treatment for diabetes affects glycemic control.
Limitation of the Study
-
- To validate our findings in the study, we require large scale, multi-center randomized control trials.
- Since this is a cross sectional study, we will follow up studies to establish the relationship between drop in lung function and control of diabetes.
- HbA1C is usually measured with high performance liquid chromatography method (HPLC) and has variable results in patients with abnormal Red cell
urnover like anaemia, Hb variants, immunosuppression, alcoholism and pregnant women39. Also, it has low positive predictive value in diagnosis of prediabetes and will need OGTT for confirmation of diagnosis40.
Conclusion
There is a definite association of pre diabetes and diabetes with asthma and the severity of irflow obstruction correlates with the HBA1C levels.
Acknowledgement
We sincerely thank the management of Apollo Hospitals for the constant support in our pursuit of excellence.
References
- Almeida R et al. DIABETIC PNEUMOPATHY. Brazilian Journal of Medicine and Human Health. 2016; 4(1).
- Kasper D, Fauci A, Hauser S et al. Harrison’s Principles Of Internal Medicine. New York: McGraw Hill Education; 2015.
- Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Emerging Risk Factors Collaboration.
- Anjana RM et al. Prevalence of diabetes and prediabetes in 15 states of India: results from the ICMR–INDIAB population-based cross-sectional study. Lancet 2017;5(8):585-596.
- American Diabetes Association. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020 Jan. 43 (Suppl1):S14- S31.
- Nidhi Bansal. Prediabetes diagnosis and treatment: A review. World J Diabetes. 2015 Mar 15; 6(2): 296–303.
- Sherwani S, Khan H, Ekhzaimy A, Masood A, Sakharkar M. Significance of HbA1c Test in Diagnosis and Prognosis of Diabetic Patients. Biomark Insights.016; 11:BMI.S38440. doi:10.4137/bmi.s38440.
- Koenig RJ, Peterson CM et al. Correlation of glucose regulation and hemoglobin A1C. N Engl J Med.1976;295:417-20
- Pitocco D, Fuso L, Conte E et al. The Diabetic Lung – A New Target Organ?. The Review of Diabetic Studies. 2012;9(1):23-35.
- . Weynaud B, Jonckheere A et al. Diabetes mellitus induces a thickening of the pulmonary basal lamina. Respiration 1999.66(1):14-19
- Walter RE, Beiser A et al. Association between glycemic state and lung function: the Framingham Heart Study. Am J Respir Crit Care Med. 2003; 167:911-6.
- Kinney GL, Black-Shinn JL et al. Pulmonary function reduction in diabetes with and without chronic obstructive pulmonary disease. Diabetes care. 2014; 37:389-95.
- Davis WA, Knuiman M, Kendall P, Grange V, Davis TM. Glycemic exposure is associated with reduced pulmonary function in type 2 diabetes: the Fremantle Diabetes Study. Diabetes Care 2004. 27(3):752-757.
- Lange P, Parner J, Schnohr P, Jensen G. Copenhagen City Heart Study: longitudinal analysis of ventilatory capacity in diabetic and nondiabetic adults. Eur Respir J 2002. 20(6):1406-1412
- McKeever TM, Weston PJ et al. Lung function and glucose metabolism: an analysis of data from the Third National Health and Nutrition Examination Survey. Am J Epidemiol 2005.161(6):546-556.
- Van der Borst et al. Diabetic pneumopathy:Evidence from a Meta-Analysis. Am J Respir Crit Care Med 179;2009:A1452
- Themeli Y, Ibro M, Dyrmishi L, Klosi J. Prevalence of bronchial asthma in patients with type 2 diabetes mellitus. Endocrine Abstracts. 2014.
doi:10.1530/endoabs.35.p355 - Ehrlich S, Quesenberry C, Van Den Eeden S, Shan J, Ferrara A. Patients Diagnosed With Diabetes Are at Increased Risk for Asthma, Chronic Obstructive Pulmonary Disease, Pulmonary Fibrosis, and Pneumonia but Not Lung Cancer. Diabetes Care. 2009;33(1):55-60. doi:10.2337/dc09- 0880
- Mueller NT, Koh WP et al. Asthma and the risk of type 2 diabetes in the Singapore Chinese Health Study. Diabetes Res Clin Pract 2013 Feb 99(2):191-199.
- Lee KH and Lee HS. Hypertensionh and diabetes mellitus as risk factors for asthma in Korean adults: the Sixth Korea National Health and Nutrition Examination Survey. Int. Health 2019;00:1-7 21. 2020 GINA Main Report – Global Initiative for Asthma – GINA.
- 2020 GINA Main Report – Global Initiative for Asthma -GINA.
- American Diabetes Association. Standards of Medical Care in Diabetes – 2020 Abridged for primary care providers. Clinical Diabetes 2020 Jan;38(1):10-38.
- Pellegrino et al. Interpretative strategies for lung function tests. European Respiratory Journal 2005 26: 948-968;
- Sofie Hansen et al. Gender differences in adult-onset asthma: results from the Swiss SAPALDIA cohort study. European Respiratory Journal 2015 46: 1011-1020
- . Mirabelli et al. Age at asthma onset and subsequent asthma outcomes among adults with active asthma. Respir Med. 2013 Dec; 107(12): 1829–1836.
- Hjellvik V et al. Body mass index as predictor for asthma: a cohort study of 118,723 males and females. European Respiratory Journal 2010 35: 1235-1242
- Perez MK et al. Metabolic asthma: Is there a link between obesity,diabetes and asthma?. Immunol Allergy Clin North Am. 2014 November; 34(4): 777–784.
- Moore et al. National Heart, Lung, and Blood Institute’s Severe Asthma Research Program. Am J Respir Crit Care Med. 2010 Feb 15; 181(4):315-23.
- Seigal S and Herzstein J. Atopy and diabetes mellitus. Journal of Allergy and Clinical immunology. 1954;25(1): 25-27
- Cardwell CR et al. A Meta-Analysis of the Association between Childhood Type 1 Diabetes and Atopic Disease. Diabetes Care 2003 Sep; 26(9): 2568-2574.
- Parasumaralu BG et al. Prevalence of bronchial asthma and its association with smoking habits among adult population in rural area. Indian J Public Health 2010; 54:165-8.
- Xinming Su et al. Prevalence of Comorbidities in Asthma and Nonasthma Patients: A Meta-analysis. Medicine (Baltimore).2016 May;95(22):e3459
- Ramachandran A, Snehalatha C, Kapur A, Vijay V, Mohan V, Das AK, et al. High prevalence of diabetes and impaired glucose tolerance in India: National Urban Diabetes Survey. Diabetologia. 2001;44:1094–101.
- Adams RJ, Wilson DH et al. Coexistent chronic conditions and asthma quality of life: a population-based study. Chest 2006;129(2):285-91.
- Caughey GE et al. Prevalence of comorbidity of chronic diseases in Australia. BMC public health. 2008;8(1):221
- Sundeep Salvi et al. Pulmonary Function Tests in Type 2 Diabetes Mellitus and Their Association With Glycemic Control and Duration of the Disease. Lung India 2013 Apr;30(2):108-12.
- Enrico Heffler et al. Bronchodilator response as a marker of poor asthma control. Respiratory Medicine 112(2016) 45-50.
- Mueller NT et al. Asthma and the risk of type 2 diabetes in the Singapore Chinese study. Diabetes Res Clin Pract 2013 February ; 99(2):192-199.
- CS L, TC A. HbA1c in the diagnosis and management of diabetes mellitus: an update. Diabetes Updates. 2020;6(1).
- Aidar Gosmanov, Jim Wan. ow Positive Predictive Value of Hemoglobin A1c for Diagnosis of Prediabetes in Clinical Practice.Am J Med Sci. 2014 Sep;348(3):191-4