694 views
K Anbananthan et al.: Etiology Underlying Pleural Effusion in Thanjavur Medical College Hospital: A Descriptive Study
Etiology Underlying Pleural Effusion in Thanjavur Medical College Hospital: A Descriptive Study
K Anbananthan1 , A Manimaran2 , G Karthick3, P Vanithamani3
1Associate Professor, 2 Senior Resident, 3 Junior Resident, Department of Thoracic medicine, Thanjavur Medical College and Hospital, Thanjavur, Tamil Nadu, India.
Abstract
Background: Pleural effusion is one of the most common signs seen in respiratory pathologies. An attempt to establish common etiologies underlying pleural effusion helps in effective management of the same.
Materials and Methods: After obtaining proper informed consent, patients presenting with pleural effusion underwent clinical examination in addition to radiological and biochemical investigations. Where needed, the diagnosis was confirmed using pleural biopsy and bacteriological analysis.
Results: Investigations confirmed tuberculosis in 23 patients, malignancy in seven cases, congestive cardiac failure in four cases, parapneumonic causes in 12 patients, hypoproteinemia in two patients, and pulmonary thromboembolism in two patients.
Angiogram: shows multiple feeders from right internal mammary artery supplying the sequestrated segment
of lung.
Treatment: Embolisation of two major feeding branches from right internal mammary artery done. Patient
became asymptomatic.
Corresponding Author: Dr. R. Ravikumar, Department of Radiology, Apollo Main Hospitals
How to cite this article: K Anbananthan, A Manimaran, G Karthick, P Vanithamani, Etiology Underlying Pleural Effusion in Thanjavur Medical College Hospital: A Descriptive Study, JAPT 2019: 2(2):44-46
Introduction
A pleural effusion represents the disruption of the normal mechanisms of formation and drainage of fluid from the pleural space. Pleural effusions are associated with diseases of varied etiologies and often carry a grave prognosis.1 Thus, a pleural effusion is abnormal excessive collection of fluid in pleural cavity resulting from excess fluid formation or decreased absorption2,3
Pleural effusion is classified as exudative and transudative on the basis of Light’s criteria. According to these criteria, all exudates have at least one of the following while transudates have none.
- Ratio of pleural fluid protein to serum protein >0.5.
- Ratio of pleural fluid lactate dehydrogenase (LDH) to serum LDH >0.6.
- Pleural fluid LDH > 2/3 of the upper limit of serum LDH.4.
Worldwide, exudative effusions are usually due to empyema, malignancy, tuberculosis, pulmonary embolism, and connective tissue diseases.4,5 In our setup, the common causes of exudative pleural effusions are tuberculosis, parapneumonic effusion, and malignancy6,7.
rapneumonic effusion, and malignancy6,7 The relative frequency of the cause of pleural effusion is known to vary in different parts of world8. However, in developing nations, infections – especially tuberculosis and parapneumonic effusions, are more prevalent9.
Objectives
The aim of this study was to find out the etiological basis of pleural effusion in patients presenting with pleural effusion in Thanjavur Medical College Hospital.
Materials and Methods
This descriptive study was conducted in the Department of Thoracic Medicine, Thanjavur Medical College Hospital, Thanjavur, over a period of 12 months from January 2018 to December 2018. Following proper clinical examination, the underlying cause of pleural effusion was established using pleural biopsy, radiological, biochemical, cytological, and bacteriological methods. Where necessary, one or combination of many investigations was used to confirm diagnosis. About 50 patients presenting with pleural effusion were involved in the study. Patients were informed about the study and proper informed consent was given by them.
Observation and Results
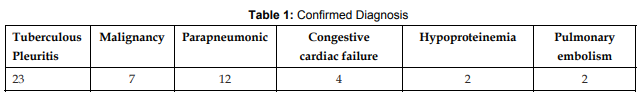
It was observed that of the 50 patients presenting with pleural effusion, investigations confirmed tuberculosis in 23 patients, malignancy in seven cases, congestive cardiac failure in four cases, parapneumonic causes in 12 patients, hypoproteinemia in two patients, and pulmonary embolism in two patients.
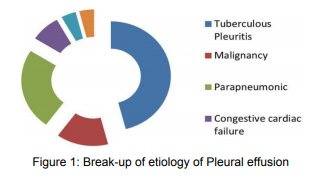
Confirmed Diagnosis Based on Combination of Investigations As seen in Table 1, based on combination of investigations, 23 cases were confirmed as tuberculous pleuritis, 7 cases were malignancies, 12 cases were parapneumonic, 4 cases were Congestive cardiac failure, 2 cases were due to hypoproteinemia and a further 2 cases were confirmed as pulmonary embolism. This is clearly illustrated in Figure 1.
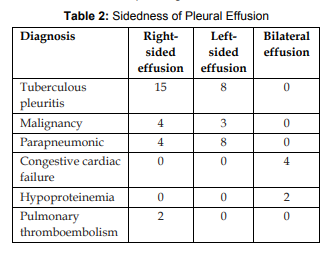
Sidedness of Pleural Effusion
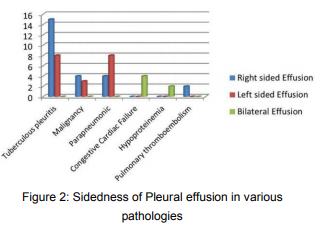
As seen in Table 2, 25 cases had right sided pleural effusion, 19 cases had left sided effusion, while only 6 cases had bilateral effusion. This is clearly illustrated in Figure 2.
Discussion
This prospective study was carried out to establish the most common causes for pleural effusion.
Of 50 patients, 31 (62%) were male, whereas 19 (38%) were female with an approximate malefemale ratio of 3:2, In our study, tuberculosis was the leading cause of pleural effusion accounting for 46% of cases. This is in concordance with many such studies conducted in developing countries such as Iraq, Ghana, and Pakistan[9-11].
Most of the patients in the present study had right-sided pleural effusion (50%) which is fairly comparable with the study of Ambethiya (right side pleural effusion – 60%) and Dambal et al. (right side pleural effusion – 58.2%).[12,13] Tuberculous pleural effusion more commonly occurs in the right side because it involves the right lung more than the left lung. Majority of pleural effusions were right sided then followed by left sided and bilateral pleural effusion. These results are comparable to a study done in Ethiopia[14].
In our study, parapneumonic effusion and malignancy respectively come next in frequency as the causes. This is similar to a study done in Lahore.[6,7] Parapneumonic effusion occurred in 24% of patients which is higher compared to results from an international study by Zablockis and Nargela[4] which showed parapneumonic causes being responsible for only 13% of effusions. Malignancy accounted for 14% of our cases which is similar to the studies done by Ambethiya (malignancy – 18%) and Dambal et al.[12,13].
Pleural effusions in patients with congestive heart failure are typically bilateral. In our study, CCF accounted for only 8% of cases. Hypoproteinemia and pulmonary thromboembolism are less frequent with each accounting for 4% of cases in our study.
Conclusion
Tuberculosis is the leading cause of pleural effusion in our study. This is similar to what is being seen in many studies conducted across developing countries. Hence, we conclude that intensive antitubercular measures may go a long way in bring down the number of patients presenting with pleural effusion.
References
1. Chowdhury PK, Ahmed S, Alam SM, Ghosh DK, Biswas SP. Etiological basis of pleural effusion in a teaching hospital. Bang Med J Khulna 2016;49:27-305.
2. Diaz-Guzman E, Dweik RA. Diagnosis and management of pleural effusions: A practical approach. Compr Ther 2007;33:237-46.
3. Frew AJ, Holgate ST. Respiratory Disease. Kumar and Clark Clinical Medicine. 6th ed. London: W.B. Saunders; 2005. p. 952-3.
4. Zablockis R, Nargela R. Diagnostic value of pleural fluid cytologic examination. Medicina (Kaunas) 2002;38:1171-8.
5. Anwar R, Faros JI. Causes of lymphocytic exudative pleural effusion as revealed by percutaneous pleural biopsy: Experience from Peshawar. Pak J Med Sci 2005;21:39-43.
6. Shaikh SJ, Memon SA. The etiology of pleural effusion in children: Hyderabad experience. Pak J Med Sci 2007;23:86- 7.
7. Anwar R, Farooqi JI. Incidence of malignancy in case of lymphocytic exudative pleural effusion, as revealed by percutaneous pleural biopsy. Med Channel 2005;11:59-61.
8. Storey DD, Dines DE, Coles DT. Pleural effusion. A diagnostic dilemma. JAMA 1976;236:2183-6.
9. Afful B, Murphy S, Antunes G, Dudzevicius V. The characteristics and causes of pleural effusions in Kumasi Ghana a prospective study. Trop Doct 2008;38:219-20.
10. Al-Alusi F. Pleural effusion in Iraq: A prospective study of 100 cases. Thorax 1986;41:492-3.
11. Khan Y, Zia SB. Etiological spectrum of exudative Pleural effusion in a tertiary care hospital based on closed pleural biopsy. Ann Pak Inst Med Sci 2011;7:133-6.
12. Kataria YP, Khurshid I. Adenosine deaminase in the diagnosis of tuberculous pleural effusion. Chest 2001;120:334-6.
13. Dambal A, Patil BS, Hegde AC. A Dissertation Submitted to Karnataka University; 1998.
14. Desalew M, Amanuel A, Addis A, Zewdu H, Jemal A. Pleural effusion: Presentation, cause and treatment outcome in a resource limited area, Ethiopia. Health 2012;4:15-19.





