694 views
Amal Johnson et al.: Phenotyping of Adult Asthmatics Visiting Pulmonology OPD of A Tertiary Care Hospital in South India
Phenotyping of Adult Asthmatics Visiting Pulmonology OPD of A Tertiary Care Hospital in South India
Amal Johnson1, Sumi M Sam2, Narasimhan R3
1Post graduate – Department of Respiratory Medicine, Apollo Hospitals, Greams Road, Chennai, India
2Physician Assistant – Department of Respiratory Medicine, Apollo Hospitals, Greams Road, Chennai, India
3Senior Consultant Pulmonologist, Apollo Hospitals, Greams Road, Chennai, India
Abstract
Background: Asthma is a chronic inflammatory airway disease with different presentation, disease
progression, and response to therapy. However, despite this recognition, the treatment approaches for
asthma have been uniformly applied irrespective of these differences. Methods: This study is a cluster analysis done in 100 consecutive patients with Asthma diagnosed according to recent GINA guidelines visiting Pulmonology OPD in Apollo Hospitals,Chennai from January 2019 to March 2019. Results: Most patients were having Atopic asthma(75%) with history of atopy, family history of asthma and elevated Total IgE. The predominant inflammatory cell type was eosinophils(35%) followed by paucigranulocytic. Breathing difficulty and wheeze were prominent symptoms. There were 16 asthmatics who smoked currently. Six patients
diagnosed as Sensitizer induced Occupational asthma (4 cement exposure, 1 coal exposure, 1 chalk dust
exposure) and 1 patient diagnosed RADS. One patient had exacerbation prone asthma and one patient had
corticosteroid dependent/resistant asthma. Conclusion: This study is an elementary attempt to categorize
diagnosed adult asthmatics into various clusters to aid in better understanding of pathophysiological process
of asthma and to tailor specific management plan for each subtype.
Keywords: Asthma, disease, phenotype, onset, atopic
Corresponding Author: Dr. Amal Johnson, Post graduate, Department of Respiratory Medicine, Apollo Hospitals, Greams Road, Chennai, India
How to cite this article: Amal Johnson, Sumi M Sam, Narasimhan R, Phenotyping of Adult Asthmatics Visiting Pulmonology OPD of A Tertiary Care Hospital in South India, JAPT 2020: 2(2):47-54
Introduction
Asthma is a heterogeneous disease characterized by respiratory symptoms such as wheeze, breathing difficulty, chest tightness and cough that vary over time, in intensity, together with variable expiratory airflow limitation1. The
chronic respiratory disease affects 1-18% of the population2-4. The episodic flare in asthma is triggered by various stimuli, such as allergens, climate change, respiratory infections, exercise and irritants. The pathophysiology of asthma is complex involving airway inflammation, intermittent airflow obstruction and bronchial hyperresponsiveness1.
Phenotype is defined as “The composite, observable characteristics of a disease, resulting from interaction between its genetic make-up and environmental influences, which are relatively stable, but not invariable, with time”. The purpose of phenotyping of asthma is to primarily understand the pathophysiology and to cluster patients that will respond to a specific treatment5.
Review of Literature
A retrospective study conducted by JL Kuhlen et al6 entitled “Identification of Asthma Phenotypes
in a Tertiary Care Medical Center” pubished in Americal Journal of Medical Sciences (2014) in 139 consecutive patients from January 2010 to May 2012 clustered patients with asthma into 5 groups based on SARP(Severe Asthma Research Program Simple Algorithm) by Moore et al7. as following 1) Pediatric onset type, atopic type light asthma 2) Pediatric onset, atopic asthma 3) Adult-onset type, primarily nonatopic type 4) Pediatric onset type, atopic type, serious asthma 5) Adult-onset type, atopic type, serious asthma.
In study entitled “Cluster analysis and clinical asthma phenotypes” published by Halder et al8 in
Americal Journal of Respiratory and critical care medicine in 2008, he categorized asthma into five phenotypes as following 1) Early onset atopic asthma 2) Obese, noneosinophilic asthma 3) Benign asthma 4) Early symptom predominant asthma 5) Inflammation-predominant asthma.
Objectives
To categorize diagnosed adult asthmatics visiting OPD of Pulmonology in a tertiary care hospital into various multiple phenotypes based on age of onset, difference in triggers, pattern of airflow obstruction, response to treatment, frequency of exacerbation, co morbidities and type of inflammation.
Materials and Methods
STUDY TYPE: Cluster analysis
SAMPLE SIZE: 100 consecutive patients with Asthma diagnosed according to GINA guidelines (2019) visiting OPD of Pulmonology
PLACE OF STUDY: Apollo Hospitals, Greams Road, Chennai
DURATION OF STUDY: January 2019 to March 2019
EXCLUSION CRITERIA: Patients were excluded if Age 12% and 200ml). Demographic and clinical data collected included Age, Gender, BMI, age of asthma onset, personal history of allergies(allergic rhinitis/atopic dermatitis), family history of asthma/allergies, smoking history, history of asthma triggers including exercise and NSAIDS use, occupation history, history of exacerbations, history of
respiratory infections, history of comorbidites, drug history including frequency of rescue inhaler use and oral corticosteroids with dose and duration, lung function by PFT, FENO, Serum neutrophil, Absolute eosinophil count and Total IgE.
The various phenotypes for categorization used in the study are
1. Atopic asthma
2. Late onset asthma including asthma in the elderly
3. Aspirin induced Asthma
4. Infection induced Asthma
5. Smoking asthmatic excluding AsthmaCOPD overlap.
6. Exercise induced Asthma
7. Exacerbation prone Asthma
8. Persistent airflow obstruction including reversible restrictive airway disease
9. Obese asthmatic excluding Asthma-COPD overlap
10. Work related asthma – occupational asthma, irritant induced asthma
11. Symptom based phenotype – SOB predominant, wheeze predominant, cough predominant
12. Corticosteroid dependent and resistant asthma
13. Inflammatory phenotype – Eosinophilic, Neutrophilic, Mixed granulocytic, paucigranulocytic
Results
Demographics
Age – Ranged from 18 to 88 with mean of 40 years
Sex – 54 males and 46 females
BMI – Ranged from 16.6 to 41.1 with average of 26.1 kg/mm<sup>2</sup>. BMI was >30 in 13 patients.
Atopic and Non Atopic Asthma
Out of the 100 patients, 75 patients were Atopic asthma and 25 were Non Atopic asthma.
In patients with Atopic asthma, childhood history of asthma in 27 patients (36%), history of atopy (Allergic rhinitis/Atopic dermatitis) in 70(93%) patients and family history of Asthma present in 36(48%) patients. There was a male predominance (60%). Total IgE was elevated in 40(53%) patients with Atopic asthma. FeNO >25 in
all patients and FeNO >50 in 5 patients. In non Atopic Asthma, there was a female predominance(70%) with FeNO > 25 in 50% of patients. Total IgE was elevated in 2 patients.
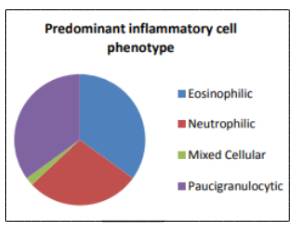
Inflammatory phenotypes
In our study, based on the serum neutrophil and absolute eosinophil count patients were classified into inflammatory cell predominant phenotype as follows
Eosinophilic – 35%
Neutrophilic – 28%
Mixed cellular – 2%
Paucigranulocytic – 35%
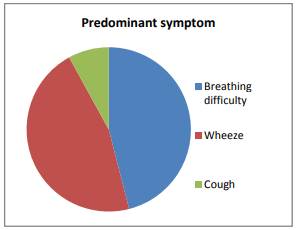
Sputum based phenotype
SOB predominant – 46%
Wheeze predominant – 46%
Cough predominant – 8%
Other relevant phenotypes
Other relevant phenotypes
There were 16 asthmatics who smoked currently. Six patients diagnosed as Sensitizer induced Occupational asthma (4 cement exposure, 1 coal exposure, 1 chalk dust exposure) and 1 patient diagnosed RADS. One patient developed
asthma post tuberculosis therapy. No exercise induced asthma and aspirin induced asthma cases were noted in the study group.
One patient had exacerbation prone asthma and one patient had corticosteroid dependent/resistant asthma.
Discussion
Asthma is a chronic inflammatory disease of the airways manifested as variable airflow obstruction with symptoms like cough, shortness of breath and chest tightness.
Characterization of asthma phenotypes is important in order to
1. better understand the etiological mechanisms of asthma
2. identify specific causes
3. guide the development of new therapeutic measures that will be effective for all asthmatic patients
4. enable better management and prevention of asthma9
Phenotypes
- Atopic asthma
- Late onset asthma including asthma in the elderly
- Aspirin induced Asthma
- Infection induced Asthma
- Smoking asthmatic excluding AsthmaCOPD overlap.
- Exercise induced Asthma
- Exacerbation prone Asthma
- Persistent airflow obstruction including reversible restrictive airway disease
- Obese asthmatic excluding Asthma-COPD overlap
- Work related asthma – occupational asthma, irritant induced asthma
- Symptom based phenotype – SOB predominant, wheeze predominant, cough predominant
- Corticosteroid dependent and resistant asthma
- Inflammatory phenotype – Eosinophilic, Neutrophilic, Mixed granulocytic, paucigranulocytic
Atopic Asthma and Non atopic asthma10
This is the most common phenotype of asthma and the onset is typically during childhood/adolescence with male predominance. It is a Th2 dominant inflammatory process with both airway and blood eosinophilia. This phenotype of
asthma usually accompanies history of allergic rhinitis/dermatitis with family history of allergy. This subtype responds well to steroids and omalizumab.
In contrast to atopic asthma, there is a late onset, female predominance without allergic sensitization. Most of the patients do not give personal or family history of allergy. This phenotype is more severe than allergic asthma and less responsive to steroids.
In our study, Out of the 100 patients included, 75 patients were Atopic asthma and 25 were Non Atopic asthma.
In patients with Atopic asthma, childhood history of asthma in 27 patients (36%), history of atopy (Allergic rhinitis/Atopic dermatitis) in 70(93%) patients and family history of Asthma present in 36(48%) patients. There was a male predominance (60%). Total IgE was elevated in 40(53%) patients with Atopic asthma. FeNO >25 in
all patients and FeNO >50 in 5 patients.
In non Atopic Asthma, there was a female predominance (70%) with FeNO > 25 in 50% of patients. Total IgE was elevated in 2 patients.
This is in concordance with the results of Moore et al7. where Atopic allergic asthma was seen in 82% of patients and almost all patients had elevated IgE. FeNO was >35 in Atopic asthma whereas it is around 10-12 in non atopic asthma. There was a female premodinance in severe asthmatics both in atopic and non atopic type.
Aspirin Induced Asthma(AIA)12
This phenotype is associated with HLA-DW2 and DPB1. The usual age of onset of symptoms is 20-35 years. Patients with ASA experience rhinorrhea and nasal congestion followed by severe bronchospasm within 2 hours after ingestion of NSAID aspirin. The prevalence of AIA is 21 % according to study by Varghese et al.30 but we did not have any patients with AIA.
Infection induced asthma13
In this phenotype, the respiratory infection influences asthma in association with onset of disease/exacerbation of disease/persistence of disease. In our study, one patient developed asthma post tuberculosis therapy.
Smoking asthmatics14, 15
Patients with asthma who smoke have severe symptoms, accelerated decline in lung function, quality of life and impaired therapeutic response to corticosteroids and theophylline. Smoking greatly modifies inflammation that is associated with asthma by various mechanisms. The prevalence of smoking in asthmatics is around 25% according to
Parasuramalu et al31 and was 16% in our study.
*Criteria for diagnosis of Asthma-COPD overlap
Major –
- Age >=40 years
- Post bronchodilator FEV1/FVC =10 pack years of tobacco or equivalent indoor or outdoor air pollution
- Documentation of asthma before age 40 years or BDR of >=400ml in FEV1
Minor –
- Documentation of allergic rhinitis or atopic disease
- BDR >=200ml and 12% from baseline values on two or more encounters
- Peripheral serum eosinophil counts >=300 cells/ml
If all major and at least one minor criteria are present, it is termed positive.
Exercise induced asthma(EIA)16
Due to evaporation of heat and water loss from the airway Starts within 3-5mins with peak bronchoconstriction occurring at 10-15 minutes.
Usually defined as >=10% decrease in FEV1 after exercise. Exercise induced asthma may be followed by refractory perior of 4 hours during which repeated exercise causes less bronchoconstriction. Symptoms may be relieved
with beta agonist therapy. The prevalence of EIA was 5-20% according to Weiler et al32. but we did not see any patients with EIA in our study.
Exacerbation prone asthma17-19
This phenotype is characterized with history of severe exacerbation requiring an emergency room visit or hospitalization atleast once in 3 months. The increased exacerbation is independent of asthma control. On stable condition, they were mild-moderate asthmatics rather than severe asthmatics.
We had one exacerbation prone asthma in our study compared to Global prevalence of 10% according to study by Stanojevic et al33.
Persistent airflow obstruction20
This is a unique phenotype characterized by reduced FEV1/FVC in a patient receiving treatment with high dose ICS during stable phase of disease for at least 4 weeks. The decreased response to short acting bronchilators is due to airway remodeling caused by chronic inflammation of airways.
We had one patient under this subtype in our study compared to the global prevalence of 7.5% according to Roche et al34.
*Risk factors for persistent airflow obstruction –
Earlier age of onset
Longer disease duration
More severe asthma
Non atopic disease/absence of rhinitis
Very frequent exacerbations
Smoking
More inflammatory cells in sputum
Greater smooth muscle hypertrophy
Importance of earlier identification of this subtype is to avoid misdiagnosis of COPD and intensive follow-up of the patients for prompt management.
Inflammatory phenotypes21
Based on the predominant inflammatory cell involved in bronchitis, asthma can be phenotyped into aucigranulocytic, eosinophilic, neutrophilic and mixed granulocytic. Eosinophilic asthma (40%) is early onset allergic asthma (Th2 mediated inflammation) and responsive to steroids and biological agents . Non eosinophic asthma is severe
asthma phenotype (Th17 mediated inflammation) characterized by poor symptom control and corticosteroid resistance.
In our study, based on the serum neutrophil and absolute eosinophil count patients were classified into inflammatory cell predominantphenotype as follows
Eosinophilic – 35%
Neutrophilic – 28%
Mixed cellular – 2%
Paucigranulocytic – 35%
In our study, 35% patients were eosinophilic and paucigranulocytic each with neutrophilic(28%) followed by mixed cellular. This is in concordance with SARP analysis by Moore et al7.
Obese Asthma22-24
Obese asthma is characterized by early onset allergic asthma complicated by development of obesity in later age. The asthma is worsened by intra abdominal and chest wall mass which causes increased pressure on the diaphragm and chest wall causing lower tidal volume hindering bronchodilator action.
According to GC forte et al35, the prevalence of BMI >30 in asthmatics is around 13% and this is in concordance with our study.
Work related asthma25-27
- Occupational asthma
1. Sensitizer induced asthma
2. RADS(Reactive airway dysfunction
syndrome)
- Work exacerbated asthma
*Occupational asthma
Sensitizer induced asthma – appears after a latency period of sensitization to the causal agent
RADS (Reactive airway dysfunction syndrome) – Clinical criteria
- Documented absence of preceding respiratory complaints
- Onset of symptoms occurred after a single specific exposure to irritant
- High concentration of irritant exposure(gas/fume/spray)
- Onset 3 months
- Symptoms simulated asthma with cough, wheeze and dyspnea predominant
- Spirometry show reversible airflow obstruction
- Methacholine challenge test was positive
- Other types of pulmonary diseases were ruled out
*Work exacerbated asthma – Patients with pre existing asthma developed worsened symptoms when exposed to occupational allergens.
In our study, six patients diagnosed as Sensitizer induced Occupational asthma (4 cement exposure, 1 coal exposure, 1 chalk dust exposure) and 1 patient diagnosed RADS. This is in concordance with results of RD Caldaeira et al where prevalence of work related asthma is 4.2%.
Symptom based phenotype28
SOB phenotype – respond well to ICS
Cough predominant – respond well to Montelukast
Wheeze predominant – respond well to ICS + Montelukast
In our study, breathing difficulty and wheeze were predominant symptoms followed by cough predominant in only 8% of patients as in study by Zedan et al28.
Corticosteroid dependent and corticosteroid resistant asthma29
Corticosteroid resistant asthma is defined as <=15% improvement in FEV1 after 2 weeks of oral prednisolone therapy 40 mg once daily. Corticosteroid dependent asthma is defined as 15-30% improvement in FEV1 after 2 weeks of oral
prednisolone therapy 40 mg once daily. Patients experience cushingoid side effects due to high dose steroid use and experience withdrawal symptoms along with worsening of symptoms and lung function after stepping down or temporary stoppage of steroid therapy.
In our study we had one patient with corticosteroid dependent asthma compared to 5-10% by SK Lukhadia et al29.
Conclusion
Asthma is not a single disease but rather a syndrome with various presentations and differential response to same treatment. There is no current guideline evidence for treatment based on phenotype so far. Future direction for research in this aspect will assist in making individualized specific treatment plan and better control of the
disease. This study is an elementary attempt to categorize diagnosed adult asthmatics into various clusters based on onset, difference in triggers, pattern of airflow obstruction, response to treatment, frequency of exacerbation, co-morbidities and type of inflammation.
Acknowledgment
We sincerely thank the management of Apollo Hospitals for the constant support in our pursuit of excellence.
References
1. 2020 GINA Main Report – Global Initiative for Asthma – GINA. https://ginasthma.org/gina-reports/
2. Masoli M, Fabian D, Holt S, Beasley R. The global burden of asthma: executive summary of the GINA Dissemination
Committee report. Allergy 2004;59:469-78.
3. Van Wonderen KE, Van Der Mark LB, Mohrs J, Bindels PJE, Van Aalderen WMC, Ter Riet G. Different definitions in childhood asthma: how dependable is the dependent variable? Eur Respir J 2010;36:48-56.
4. Godar M, Blanchetot C, de Haard H, Lambrecht B, Brusselle G. Personalized medicine with biologics for severe type 2 asthma: current status and future prospects. MAbs. 2017;10(1):34-45.doi:10.1080/19420862.2017.1392425
5. Lai CKW, Beasley R, Crane J, Foliaki S, Shah J, Weiland S, International Study of A, et al. Global variation in the prevalence and severity of asthma symptoms: phase three of the International Study of Asthma and Allergies in
Childhood (ISAAC). Thorax 2009;64:476-83
6. Kuhlen JL et al. Identification of Asthma Phenotypes in a Tertiary Care Medical Center. Am J Med Sci.2014;348(6):480-485.
7. Moore et al. National Heart, Lung, and Blood Institute’s Severe Asthma Research Program. Am J Respir Crit Care
Med. 2010 Feb 15; 181(4):315-23.
8. Halder PH, Pavord ID, Shaw DE et al. Cluster analysis and clinical asthma phenotypes. Am J Resp Crit Care Med.
2008;178:218-24.
9. Pembrey L, Barreto ML et al. Understanding asthma phenotypes: the World Asthma Phenotypes(WASP). ERJ Open Res 2018; 4: 00013-2018.
10. Saglani S, Bush A. Asthma, Atopy, and Airway Inflammation. Am J Respir Crit Care Med. 2008;178(5):437-
438. doi:10.1164/rccm.200805-796ed
11. Wüthrich B (ed): The Atopy Syndrome in the Third Millennium.Curr Probl Dermatol. Basel, Karger, 1999, vol
28, pp 129-134
12. Hamad AM, Sutcliffe AM, Knox AJ. Aspirin-induced asthma: clinical aspects, pathogenesis and management.
Drugs. 2004;64(21):2417-32.
13. Darveaux J, Lemanske RF et al. Infection related asthma. J Allergy Clin Immunol Pract. 2014 Nov-Dec; 2(6): 658–663.
14. Thomson NC, Chaudhuri R et al. Asthma and cigarette smoking. Eur Respir J 2004;24: 822-833.
15. Chatkin J, Dullius C. The management of asthmatic smokers. Asthma Res Pract. 2016;2(1). doi:10.1186/s40733-
016-0025-7
16. SD Giacco, D Firinu et al. Exercise and asthma: an overview. Eur Clin Respir J 2015;2:10.3402
17. NJ Sathish et al. Repeated exacerbation of asthma: An intrinsic phenotype of uncontrolled asthma. Lung India
2019 March;36(2):131-138
18. Corren J. Exacerbation-prone asthma-intrinsic to severe disease or a unique phenotype?. Clinical & Experimental Allergy. 2014;44(2):152-153. doi:10.1111/cea.12256
19. RJ Loymans et al. Exacerbation-prone Asthma: A seperate bioclinical Phenotype. American Journal of Respiratory and Critical Care Medicine, 195(3), pp. 275–277
20. Persistent Airway Obstruction in Asthma. Am J Respir Crit Care Med. 2013;187(1):1-2. doi:10.1164/rccm.201211-1966ed
21. Sarath S, P Nair. Asthma Endotypes and an overview of targeted therapy for Asthma. Frontiers in Medicine
2017;4:158
22. Baffi C, Winnica D, Holguin F. Asthma and obesity: mechanisms and clinical implications. Asthma Res Pract.
2015;1(1). doi:10.1186/s40733-015-0001-7
23. Dixon A, Poynter M. Mechanisms of Asthma in Obesity. Pleiotropic Aspects of Obesity Produce Distinct Asthma
Phenotypes. Am J Respir Cell Mol Biol. 2016;54(5):601-608.doi:10.1165/rcmb.2016-0017ps
24. Baffi C, Winnica D, Holguin F. Asthma and obesity: mechanisms and clinical implications. Asthma Res Pract.
2015;1(1). doi:10.1186/s40733-015-0001-7
25. Vandenplas O, Malo J. Definitions and types of workrelated asthma: a nosological approach. European
Respiratory Journal. 2003;21(4):706-712. doi:10.1183/09031936.03.00113303
26. Dykewicz et al. Occupational asthma: Current concepts in pathogenesis, diagnosis and management. Journal of
allergy and clinical immunology.March 2009;123(3):519-528
27. M Brooks S. Irritant-Induced Asthma and Reactive Airways Dysfunction Syndrome (RADS). Journal of Allergy
& Therapy. 2014;05(03). doi:10.4172/2155-6121.1000174
28. Zedan M, Attia G, Zedan M et al. Clinical Asthma Phenotypes and Therapeutic Responses. ISRN Pediatr.
2013;2013:1-7. doi:10.1155/2013/824781
29. SK Ludadia. Steroid Resistant Asthma. Journal of assofication of physicians of India. 2014; 62:38-40.
30. Varghese, M., & Lockey, R. F. (2008). Aspirin-Exacerbated Asthma. Allergy, Asthma & Clinical Immunology, 4(2), 75.
31. Parasuramalu B G, Huliraj N, Rudraprasad B M, Prashanth Kumar S P, Gangaboraiah, Ramesh Masthi N R. Prevalence
of bronchial asthma and its association with smoking habits among adult population in rural area. Indian J Public Health 2010;54:165-8
32. Weiler JM, et al. American Academy of Allergy, Asthma & Immunology Work Group report: exercise-induced asthma. J. Allergy Clin. Immunol. 2007;119:1349–1358. doi:10.1016/j.jaci.2007.02.041.
33. Stanojevic S, Moores G, Gershon AS, Bateman ED, Cruz AA, et al. Global asthma prevalence in adults: Findings
from the cross-sectional world health survey. BMC Public Health. 2012;12:204.
34. Roche, N., Dalmay, F., Perez, T., Kuntz, C., Vergnenegre, A., Neukirch, F., Huchon, G. (2008). Impact of chronic airflow obstruction in a working population. European Respiratory Journal, 31(6), 1227–1233.
35. GC Forte et al. Prevalence of obesity in asthma and its relations with asthma severity and control. rev assoc med bras. 2013;59(6):594–59





